Dr Peter Houghton – Novel Therapeutics For Childhood Solid Tumours
Dr Peter Houghton’s group implements preclinical trials to identify new drugs that may be effective and less toxic treatments against childhood cancers. From patient-derived xenografts in immunodeficient mice to utilising canine cancer patients as models, they have identified over 80 new drugs or drug combinations for the treatment of these diseases.
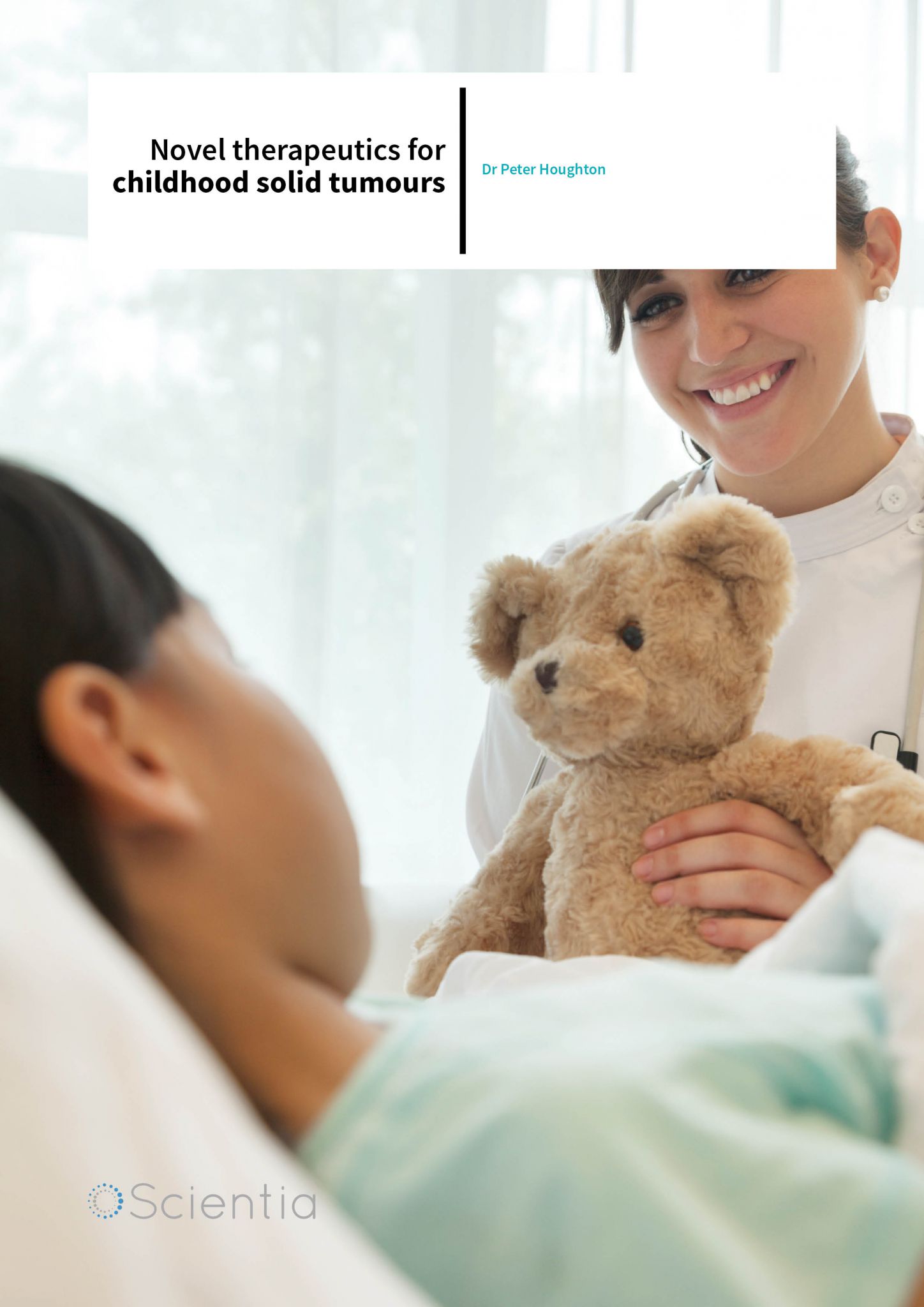
Solid tumours in children
Approximately 12,400 cases of cancer are diagnosed in the U.S. annually in individuals under 20 years of age. Solid tumours comprise approximately 30% of all childhood cancers. There are critical and unique aspects surrounding the study of paediatric tumours as compared to adult tumours, one of which is that many of the most common paediatric cancers are rarely observed in adults. Some of these include osteosarcoma, rhabdomyosarcoma, Ewing’s sarcoma, retinoblastoma, Wilms’ tumour, and neuroblastomas. Complicating the discovery of novel therapeutic options for these tumours are their low incidence rate, exponentially increasing the time for successful clinical trials to take place. For instance, only approximately 250 cases of Ewing’s sarcoma are diagnosed in the US annually. Currently available chemotherapeutic or surgical protocols, while curative in the majority of patients, are often toxic and invasive, calling for further advancement in the field of therapies to treat childhood cancers.
Dr Peter Houghton, a researcher at the University of Texas Health Science Center, focuses on improving treatments for these paediatric solid tumours. Since the 1940s, when the first chemotherapeutic and radiation protocols that aimed to improve the prognosis of cancer patients were implemented, researchers have been striving to develop new approaches to battle neoplasia. Frequently used chemotherapeutic agents in paediatric cancers currently include vincristine, cyclophosphamide, cisplatin, irinotecan and others. While many protocols using these agents in combination with radiation therapy have dramatically improved cure rates, many of them have deleterious side effects, including marked immunosuppression leading to infections, clotting disorders, malnutrition, and long-term sequelea such as cardiac dysfunction and for survivors of brain tumours, cognitive impairment. These side effects may be especially significant in young children where brain development is ongoing. Fewer than 15% of anti-cancer therapies indicated for use in adults are also approved for use in children, further limiting drug options for practicing oncologists. Further, chemotherapeutic or radiation therapy is often coupled with invasive surgical resection, providing increased opportunities for secondary post-operative bacterial infection and slow healing times. While overall national cure rates for childhood cancers is 70%, and 5-year disease-free survival is approaching 80%, the success rate is not nearly as high for patients with advanced disease or where the cancer has metastasised. It is for these patients where exploration of alternative therapeutic protocols is required. However, as a consequence of the rarity of these cancers, the high cure rate, and the prolonged disease-free survival of current clinical treatment, relatively few patients are eligible for new experimental therapies. Thus, approaches to develop preclinical models of paediatric cancer that can identify effective new agents and combinations have been a focus of Dr Houghton’s research.
Patient-derived xenografts
One recent area of research has been the development and characterisation of patientderived xenografts (PDX). Xenografts are the implantation of tissues or organs from the donor of a different species from the recipient. Many xenotransplantation efforts have focused on the transplant of tissues and organs from pigs and non-human primates into human patients. However, Dr Houghton’s work focuses on the use of patient derived tumour xenografts. These are created by transplanting cancerous tissues directly from the patient into immunodeficient mice to more accurately mimic the physiologic environment and histopathology appreciated in patient tumours. For these studies, it is crucial the mice do not have functioning immune systems so that they do not reject the transplant. Several strains of immunodeficient mice exist for these studies, including athymic nude mice, severely compromised immune deficient (SCID) mice, and non-obese diabetic SCID (NOD-SCID) mice. After the tumour specimens have successfully grown, they are harvested and implanted into further generations of mice to study the molecular fidelity of the graft, as well as its biologic characteristics. These models have also been used extensively to identify novel therapeutic agents for treating childhood cancers.
Dr Houghton’s research has led to the development of approximately 100 PDX models representing a multitude of childhood cancer types and the subsequent development of several preclinical drugs used in clinical trials. Using these PDX models, they have identified a class of drug (camptothecins) as successful in the regression of sarcomas and neuroblastomas, as well as other cancer types. One of the camptothecin drugs, irinotecan, is now incorporated into many protocols for the treatment of childhood solid tumours worldwide, exemplifying the translation of preclinical results to clinical trials and effective clinical outcomes. To date, Dr Houghton and his group have published over 66 papers on the activity, metabolism, and clinical relevance of camptothecins in paediatric solid tumours.
Dr Houghton’s research has led to the development of approximately 100 PDX models representing a multitude of childhood cancer types and the subsequent development of several preclinical drugs used in clinical trials.

The importance of the insulin growth factor axis in neoplastic inhibition
Early studies using PDX models identified the insulin-like growth factor axis as important for tumour progression in several types of childhood sarcoma. In one study, Dr Houghton’s lab successfully inhibited type 1 insulin-like growth factor receptor (IGF-1R), a common receptor often actively involved in signalling in childhood sarcomas, in conjunction with rapamycin, an immunosuppressive drug that blocks mammalian Target of Rapamycin complex 1 (mTORC1), downstream of IGF-1R. Capitalising on the antitumour properties of CP-751, 871 (Figitumumab), a human antibody blocking IGF-1R ligand binding, in concert with effects of rapamycin (also known as sirolimus), Dr Houghton and colleagues demonstrated a synergistic effect on tumour cell death in 5 of 13 xenograft models examined and elicited tumour remission in rhabdomyosarcoma and osteosarcoma models.
Currently, Dr Houghton’s lab is focusing on identifying resistance mechanisms to therapeutics targeting the insulin growth factor axis and further identifying the signalling pathways in the maintenance of malignant phenotypes. It is unclear whether or not these drugs lose efficacy due to the selection of a pre-existing clone within the patient or through a therapyinduced mutation. Further, Dr Houghton and colleagues aim to identify biomarkers that may allow for future patient stratification based on potential for the presence of drug resistance. Expression profiling of these xenografts may allow for this in the future.
The Houghton lab collaborates with individuals from The Ohio State University, Tufts University and University of Maryland on this project. Resources provided by the Program Project Grant to Greehey Children’s Cancer Research Institute are comprised of three cores. One core, based at OSU provides communication and biostatistical support and another, at GCCRI provides the xenograft and cell line for in vitro and in vivo mouse models. The third, at Tufts University, the Comparative Animal Core, employs a translational approach using canine osteosarcoma patients for drug evaluation. This core provides canine tumour specimens and expertise in histopathologic examination of the tumours. They also evaluate the novel therapeutics of interest in these animals.
Dr Houghton’s lab successfully inhibited type 1 insulin-like growth factor receptor (IGF-1R), a common receptor often actively involved in signalling in childhood sarcomas, in conjunction with the immunosuppressant rapamycin.
The Paediatric Preclinical Consortium
Building upon the in vitro and in vivo mouse model studies Dr Houghton’s group has focused on, the National Cancer Institute implemented the Pediatric Preclinical Testing Program (PPTP). The PPTP comprised a consortium of investigators in the US and Australia that used PDX models for testing new therapeutic agents against not only childhood solid tumours, but also brain tumours and acute lymphoblastic leukaemia models. To date, over 80 therapeutic agents have been tested against 83 models of childhood cancers and these studies have successfully identified drugs and drug combinations currently in clinical trial. New models are characterised via exome sequencing, gene expression profiling and single nucleotide polymorphisms. Agents and combinations that have moved into clinical trials, based in part on PPTP studies, include IGF-1R-targeted antibodies, the combination of a rapamycin derivative with standard cytotoxic chemotherapy, as well as other biologic and small molecule agents.
By continuing to collaborate with other cancer research groups worldwide through open web portals, genomic data spanning numerous cell lines and stemming from both in vivo and in vitro studies may be centralised in one location. Several open web portals exist providing cancer genomic data to the public, much of it from the Tumor Cancer Genome Atlas (TCGA). Using these resources, researchers may quickly access information on a gene of interest, neoplastic pathways, and cancer therapy sensitivity or resistance patterns. One use of relating tumour sensitivity to genomics databases is to identify the underlying mechanism for ‘exceptional responders’, those rare tumours that demonstrate a dramatic response to a drug. Such genomic signatures may then be used as biomarkers to identify patients who may benefit from that treatment. Breast cancer with biallelic mutations in BRCA genes, for example respond better to PARP inhibitors.
Brain tumours
An example of an ‘exceptional responder’ was identified in the PPTP screen. Specifically, an astrocytoma PDX model completely regressed upon treatment with the MEK inhibitor, selumetinib (AZD6244). Low-grade astrocytomas are associated with BRAF activation and/or mutation and are the most commonly diagnosed neoplastic disease of the central nervous system in children. Utilising genotyping and expression profiling through deep sequencing, Dr Houghton and his group are using astrocytoma xenografts as a model to investigate the possibility of BRAF mutation as a potential drug target. More recently selumetinib, and a BRAF inhibitor dabrafenib have shown promising clinical activity against low-grade glioma in children. This has indications for clinical trials examining novel therapeutics against paediatric astrocytomas in the future. While most of these astrocytomas are considered low-grade tumours, many are inoperable and require chemotherapy and radiation as surgical excision is not a viable option due to the fragile structures frequently involved within or adjacent to the tumour. For this reason, adjuvant or combination therapy is frequently indicated, namely chemotherapy and/or radiation therapy. Preliminary results in the astrocytoma model indicate that selumetinib may enhance radiation sensitivity selectively in tumours with BRAF aberrations. Potentially, this may allow lower doses of radiation therapy to be used in curative treatment with decreased longterm toxicity which is largely a consequence of radiation treatment.
Future work
Dr Houghton and his group of graduate students and post-doctoral students will continue making strides towards the identification of novel drugs or drug combinations in the treatment of paediatric solid tumours and other neoplastic diseases, such as acute lymphoblastic leukaemia. With new advances in whole genome and exon sequencing, the identification of biomarkers using patient derived xenografts to monitor potential efficacy or resistance will help accelerate these drugs into clinical trials.
Meet the researcher
Dr Peter Houghton
Director, Greehey Children’s Cancer Research Institute
University of Texas Health Science Center at San Antonio
San Antonio
USA
Dr Peter Houghton completed his Bachelor’s degree at the University of Bradford in the UK, where he studied pharmacology. He then assumed a PhD position in biochemistry and pharmacology at the Institute of Cancer Research at the University of London. He was Chair, Molecular Pharmacology at St. Jude Children’s Research Hospital for 17 years and currently serves as the Director of the Greehey Children’s Cancer Research Institute (GCCRI), and holder of the Greehey Distinguished Chair for the Children’s Cancer Research Institute. Primarily, Dr Houghton’s group aims to elucidate the mechanisms of tumor initiation and progression in children and uses this knowledge to identify less toxic drugs with higher cure rates. Houghton has largely been funded through the NIH for over 30 years and has directed NIH program grants for over 25 years.
CONTACT
T: (+1) 210 562 9161
E: HoughtonP@uthscsa.edu
W: http://ccri.uthscsa.edu/PHoughton.html
KEY COLLABORATORS
Denis Guttridge, Ph.D. Ohio State University
Jiayuh Lin, Ph.D. University of Maryland
Cheryl London, DVM, Ph.D. Tufts Unversity
FUNDING
NIH
REFERENCES
H Cam, JB Easton, A High and PJ Houghton, mTORC1 signaling under hypoxic conditions is controlled by ATM-dependent phosphorylation of HIF-1ạ, Molecular Cell, 2010, 40, 509–520.
B Geier, D Kurmashev, RT Kurmasheva and PJ Houghton, Preclinical childhood sarcoma models: drug efficacy biomarker identification and validation, Frontiers in Oncology, 2015, 5, 1–15.
RT Kurmasheva, L Dudkin, C Billups, LV Debelenko, CL Morton and PJ Houghton, The insulin-like growth factor-1 receptor-targeting antibody, CP-751,871, suppresses tumor-derived VEGF and synergizes with rapamycin in models of childhood sarcoma, Cancer Research, 2009, 69, 7662–7671.
C Shen and PJ Houghton, The mTOR pathway negatively controls ATM by up-regulating miRNAs, Proceedings of the National Academy of the Sciences, 2013, 110, 11869–11874.
KN Thimmaiah, JB Easton and PJ Houghton, Protection from rapamycin-induced apoptosis by insulin-like growth factor-I is partially dependent on protein kinase C signaling, Cancer Research, 2010, 70, 2000–2009.