Dr Stephen Pandol – Understanding the Causes of Pancreatic Disease to Improve Patient Outcomes
The incidence of pancreatic disease, including pancreatitis and pancreatic cancer, is on the rise, but currently, preventative measures and effective treatments are scarce. Dr Stephen Pandol at the Cedars-Sinai Medical Center in Los Angeles is working to change this. Dr Pandol carries out broad and far-reaching research, ranging from how lifestyle factors impact pancreatic disease to the molecular and cellular mechanisms behind pancreatic cancer resulting from obesity. His dedicated work has led to significant progress in the field and is driving forward the potential for better patient outcomes.
The Function of the Pancreas
The pancreas is a roughly hand-sized organ found just behind the stomach. It has an integral role in both exocrine function during digestion and endocrine function for blood sugar regulation.
Its exocrine function involves creating around 200 ml of digestive juice daily, which is packed with enzymes like protease, lipase and amylase to break down proteins, fats and sugars. The juices travel through the ducts in the pancreas to the duodenum in the small intestine where they get to work digesting meal nutrients for absorption.
Pancreatic hormones for endocrine function are also synthesised in the organ but are released into the bloodstream to send signals to other organs. One hormone, insulin, is synthesised by pancreatic cells called beta cells, which make up around 75% of the hormone cells in the pancreas. When an increased level of glucose is detected in the blood after eating, insulin sends messages for it to be stored in the liver where it can be used later. Glucagon is another hormone that signals for this stored sugar to be released by the liver when blood glucose levels are low. It is made in alpha cells, which comprise around 20% of the hormone cells.
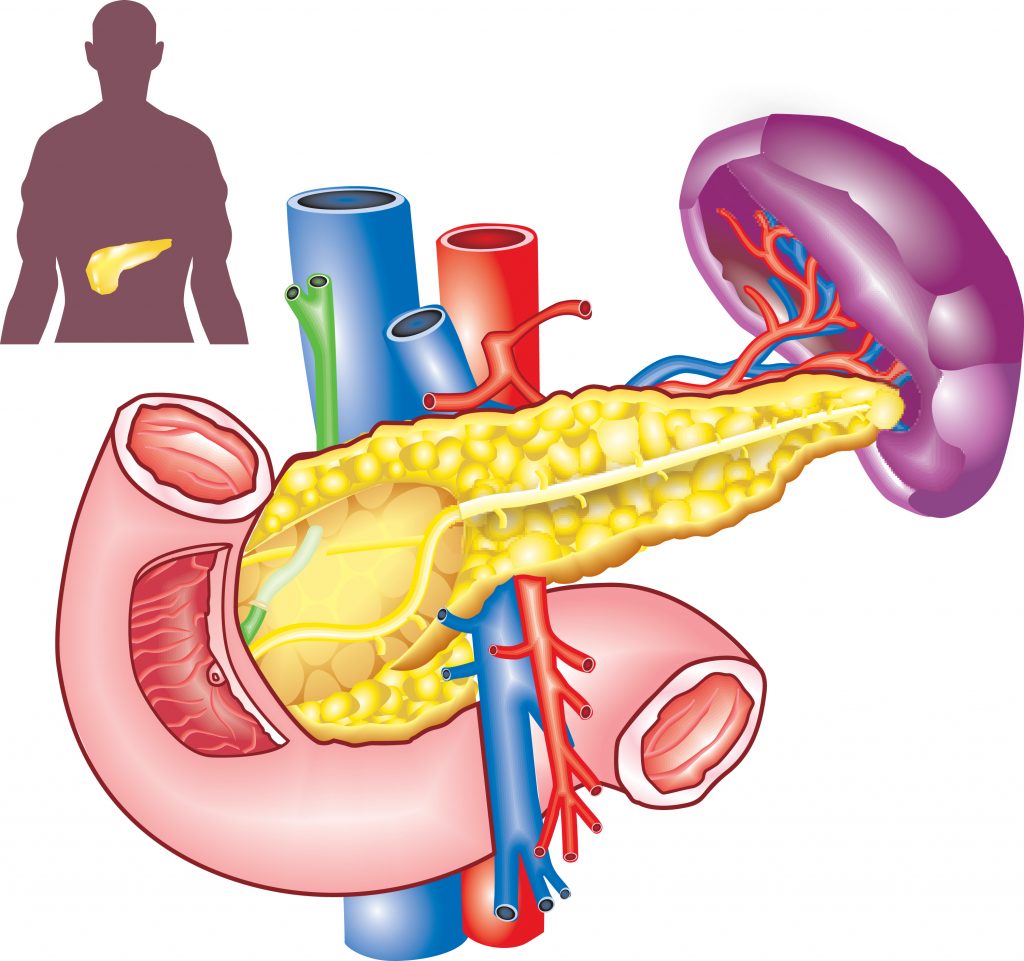
Illustration of the pancreas
Diseases of the Pancreas
A well-known pancreatic disease is diabetes. Type 1 diabetes is an autoimmune disease that results in the destruction of insulin-producing beta cells and a subsequent inability to regulate blood sugar. On the other hand, type 2 diabetes is often a consequence of obesity. Constant high blood sugar levels cause cells (such as in the liver) to become resistant to insulin and so increasingly higher amounts of the hormone are produced to try and fulfil the need. However, this overproduction is unsustainable and eventually, beta cells burn out and can’t make enough insulin. Both Type 1 and Type 2 diabetes have the outcome of elevated blood sugar which can be remedied through medications, and for type 2 diabetes, diet management.
Pancreatitis is a painful inflammation of the pancreas caused by digestive enzymes attacking the organ itself. It can be caused by gall stones or excessive alcohol consumption and may lead to malnutrition and weight loss.
Another health issue that can arise within the pancreas is pancreatic cancer. Around 95% of pancreatic cancers start in exocrine cells and are called pancreatic adenocarcinomas. It causes a reduction in the number of digestive enzymes produced, and as a result, loss of appetite and weight loss are common indicators of the disease. Risk factors for pancreatic cancer include obesity, diabetes smoking and chronic forms of pancreatitis.

Pancreatic Adenocarcinoma is a Significant Health Dilemma
In a world where overall deaths due to cancers are decreasing, incidence and deaths from pancreatic cancer are still on the rise. In the last 30 years, the five-year survival rate has shockingly only increased from 3% to 7%. Contributing to this poor figure is the fact that only 20–30% of pancreatic cancer patients are eligible for resection (removal of the tumour) because the disease is often only detected after it has widely spread. This surgery is currently the best chance of cure and even these patients can relapse. Inadequate understanding of markers that could lead to earlier diagnosis and ineffective treatment regimens both contribute to these harsh outcome numbers.
However, determined scientists like Dr Stephen Pandol are leading the way in progressing understanding of pancreatic disease. At the Cedars-Sinai Medical Center in Los Angeles, Dr Pandol explores the underlying mechanisms of pancreatic disease and cancer, with a particular focus on lifestyle factors. The overarching goal of this work is to develop more effective therapeutics.

Obesity as a Pancreatic Cancer Risk
Diet-induced obesity and chronic forms of pancreatitis are frequently connected with the development of cancer, including pancreatic adenocarcinoma. However, the processes that lead from them to cancer are unclear. Working with colleagues at Cedars-Sinai Medical Center and the University of California, Los Angeles (UCLA), Dr Pandol examined these associations using mice.
They used wildtype mice, which are mice with standard genetic material, and KC mice, which are mice with a pancreas-specific oncogenic mutation in their Kras gene. Both mice were fed a high-fat and high-calorie diet so that they developed diet-induced obesity. The wildtype mice exhibited the expected weight gain and insulin resistance. Dr Pandol and his team focused on the role of cells in the microenvironment of the pancreas known as pancreatic stellate cells (PaSCs). These cells mediate the development of fibrosis and inflammation that occurs in pancreatic cancer and interact with early pancreatic cancer cells to facilitate the progression and metastasis of the cancer. All of these factors are linked to the acceleration of the development of pancreatic adenocarcinoma tumours, which implies that pancreatic stellate cells have an important role in promoting obesity-induced pancreatic tumours.
Dr Pandol and the team found that numerous signals are a crucial element in activating the pro-cancer effects of PaSCs. These included extracellular signals such as the cytokines IL-4/IL-13 and the hormones insulin and insulin-like growth factor 1 (IGF1). Intracellular signals are also needed – transcription factors like STAT3 and enzymes like mTOR/Akt. By regulating the immune system to favour the tumour, preventing apoptosis (cell death) and promoting tumour cell growth, these signals allow PaSCs to continue supporting tumour progression.
The team also analysed large databases of people who had experienced pancreatic adenocarcinoma, and specifically, patients who received simvastatin as a therapy. Simvastatin is a member of a group of drugs that lower cholesterol, called statins. It can be prescribed to prevent cardiovascular issues or given as a treatment for type 1 and type 2 diabetes. Patients in this retrospective analysis showed better disease-free survival rates after tumour resection if they took simvastatin.
Summarising these studies, Dr Pandol hypothesises that obesity produces unique signals in the microenvironment of developing pancreatic adenocarcinomas, inducing observable alterations in PaSCs. The result is the production of signals that promote rapid growth and resistance in cancer cells, and a shift in the immune response to a pro-tumour state. In other words, obesity creates a much more favourable environment for cancer cells to survive and spread.

Building on the Findings
This work is only the beginning of what Dr Pandol plans to achieve and he has specific aims for his future work. He plans on studying the effects of eliminating activated PaSCs at various stages of pancreatic adenocarcinoma development in KC mice who will be fed normal and high obesity-inducing diets. He will also continue work to uncover how different cell types ‘talk’ to each other within a tumour microenvironment. This will provide insight into the role of PaSCs in tumour development.
Additionally, determining which pathways obesity impacts to promote cancer formation through PaSCs is important. Further studying how the previously mentioned signals (such as IL-4) and their pathways respond to obesity will shine light on how processes leading to the activation of PaSCs are involved in cancer.
Simvastatin and another drug known as metformin are also interesting leads to explore. Metformin reduces the amount of sugar being released from the liver whilst improving insulin’s function to remove sugar from the blood. This makes it a common and effective way of reducing blood glucose levels for patients with type 2 diabetes. Dr Pandol and his team will study how these drugs affect the activation of PaSCs and tumour progression in KC mice. The findings will be used to improve preventative strategies for at-risk patients, and are likely to play an essential role in improving pancreatic cancer survival rates.
Contributing to the Field
All of this is just a fraction of the work that Dr Pandol has headed and contributed to over his extensive career in pancreatic disease research. He has studied how stressors on pancreatic organelles lead to pancreatitis, investigated how pancreatic disease diagnosis can be improved through developing magnetic resonance imaging techniques, and much more. Upcoming studies will look into how lifestyle factors such as alcohol consumption and smoking, lead to pancreatitis so that clinical recommendations can be updated. His work is proving to be vital for broadening and deepening our understanding of pancreatic disease so that patient outcomes can be vastly improved.
Short on time? Learn quickly by watching this animation
Reference
https://doi.org/10.33548/SCIENTIA664
Meet the researcher

Dr Stephen Pandol
Cedars-Sinai Medical Center
Los Angeles, CA
USA
Dr Stephen Pandol completed his Bachelor of Science in Biochemistry at the University of California, Davis, and went on to achieve his Doctor of Medicine degree at St. Louis University in Missouri. Dr Pandol is extremely active in his clinical and research work on pancreatic biology and disease, and as part of his remit, directs the Basic and Translational Pancreatic Research at Cedars-Sinai Medical Center He also co-directs the UCLA Center for Excellence in Pancreatic Diseases, the Southern California Research Center for Alcoholic Liver and Pancreatic Diseases and the NIH-sponsored Consortium on Chronic Pancreatitis, Diabetes and Pancreatic Cancer. In addition, he is a Staff Physician, Professor of Medicine and past President of the American Pancreatic Association, from whom he received a Lifetime Achievement Award in 2015.
CONTACT
E: stephen.pandol@cshs.org
W: https://www.cedars-sinai.edu/research/labs/pandol.html
Twitter: @CedarsSinaiMed
FURTHER READING
L Wang, S Gaddam, N Wang, et al., Multiparametric Mapping Magnetic Resonance Imaging of Pancreatic Disease, Frontiers in Physiology, 2020, 11.
Q Wei, L Qi, H Lin, et al., Pathological Mechanisms in Diabetes of the Exocrine Pancreas: What’s Known and What’s to Know, Frontiers in Physiology, 2020, 11, 570276.
A Habtezion, AS Gukovskaya, SK Pandol, Acute Pancreatitis: A Multifaceted Set of Organelle and Cellular Interactions, Gastroenterology, 2019, 156(7), 1941–1950.
RT Waldron, Y Chen, H Pham, et al., The Orai Ca2+ channel inhibitor CM4620 targets both parenchymal and immune cells to reduce inflammation in experimental acute pancreatitis, The Journal of physiology, 2019, 597(12), 3085–3105.
DK Andersen, CE Forsmark, SJ Pandol, The Agenda for Accelerating Pancreatic Research, Pancreas, 2018, 47(10), 1177–1179.
M Edderkaoui, C Chheda, B Soufi, et al., An Inhibitor of GSK3B and HDACs Kills Pancreatic Cancer Cells and Slows Pancreatic Tumor Growth and Metastasis in Mice, Gastroenterology, 2018, 155(6), 1985–1998.

Want to republish our articles?
We encourage all formats of sharing and republishing of our articles. Whether you want to host on your website, publication or blog, we welcome this. Find out more
Creative Commons Licence
(CC BY 4.0)
This work is licensed under a Creative Commons Attribution 4.0 International License. 
What does this mean?
Share: You can copy and redistribute the material in any medium or format
Adapt: You can change, and build upon the material for any purpose, even commercially.
Credit: You must give appropriate credit, provide a link to the license, and indicate if changes were made.
More articles you may like
Probing Electron Dynamics in the Ultrafast Regime
In the atoms that make up the matter around us, negatively charged particles called electrons have properties such as spin and orbital angular momentum. Researchers at Martin Luther University Halle-Wittenberg have developed a theoretical framework which allows them to simulate the dynamics of the spin and orbital angular momentum of electrons in materials when probed with an ultrafast laser pulse. Using this framework, they are able to simulate different materials and improve our understanding of dynamics on an atomic scale.
Seeing Beneath the Surface: Exploring Deltaic Reservoirs with Augmented Reality
In the Aínsa Basin of the Spanish Pyrenees, the Mondot-1 well was drilled, cored, and fully logged to capture a detailed record of a long-buried ancient river delta system. Dr. John D. Marshall, Dr. Jürgen Grötsch, and Dr. Michael C. Pöppelreiter with co-workers at Shell International used this core to trace how sediments once flowed across the landscape, and were deposited under shifting tectonic conditions. The team employed augmented reality and interactive virtual displays; these innovative tools offer new ways to explore subsurface depositional systems, and are particularly useful in locations where physical access to the core is difficult, or no longer possible.
Dr Jim Wu | Ziresovir Offers New Hope for Treating Respiratory Syncytial Virus Infections
Respiratory syncytial virus (RSV) causes respiratory tract infections in children and adults. While for many patients the outcomes of infection are mild, for others, infection can prove fatal, and there is a lack of effective treatments. Dr Jim Wu from the Shanghai Ark Biopharmaceutical Company in China carries out his vital research to develop new, safe, and effective treatments to tackle this killer.
Dr Sandra Grumelli | The Importance of the Choline in Chronic Lung Infections
People with chronic lung conditions like COPD and cystic fibrosis are vulnerable to lung infections caused by the bacterium Pseudomonas aeruginosa. These infections are often difficult to treat and can cause sudden worsening of symptoms, known as flare-ups or acute exacerbations. While we know P. aeruginosa triggers inflammation and damage in the lungs, much less is understood about how exactly it causes these flare-ups, or how it survives in such a harsh environment. Dr Sandra Grumelli from the Center of Investigations of Respiratory Diseases in Argentina, has explored the role of a common molecule called choline which is released during infection. Using a combination of mouse models and laboratory experiments, she has discovered that choline not only makes breathing harder, it also helps P. aeruginosa adapt to and persist in the lungs. Her research opens up new possibilities for tackling chronic infections by targeting the bacteria’s energy use and the way it responds to its environment.