Dr Abigail Raffner Basson | Inflammatory Bowel Disease: The Influence of Our Microbiota and the Impact of Diet
Chronic inflammation within the digestive tract is known as inflammatory bowel disease. While the incidence is increasing, unfortunately, we do not yet fully understand what causes the condition or have a cure for it. Dr Abigail Raffner Basson from Case Western Reserve University is investigating the underlying mechanism of this disease and conducting clinical research into how diet can be used to control the debilitating, lifelong symptoms.
A Lifelong Condition
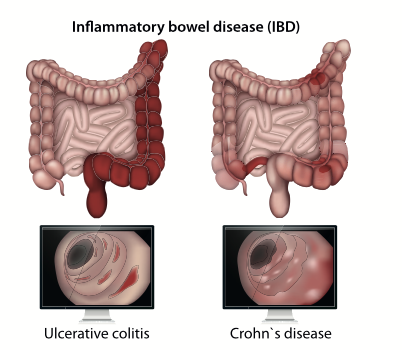
Inflammatory bowel disease (IBD) is a lifelong medical condition affecting almost 10 million people around the world. It is a chronic condition which has severe symptoms that often significantly impact the patient’s quality of life. IBD occurs when there is chronic inflammation within the digestive tract, and includes two specific conditions: Crohn’s disease and ulcerative colitis.
Ulcerative colitis affects the colon (large intestine), whereas Crohn’s disease can affect any part of the digestive tract. Both conditions involve alternating periods of inflammation (known as flare-ups) and remission periods with no symptoms. The inflammation can lead to long-term damage to tissues and structures within the digestive tract.
The exact cause of IBD is not yet known, but it is thought to originate with problems in the immune system, and it is likely genetics are involved as you are much more likely to get IBD if a close relative also has the condition. Differences have been found in the types of bacteria found in the guts of people with and without IBD, suggesting these organisms (known as the gut microbiota) could play a role in the development and prevention of IBD.
Common symptoms of IBD include recurring or bloody diarrhoea, pain, cramps, stomach bloating, weight loss and extreme tiredness. There is currently no cure for either Crohn’s disease or ulcerative colitis, and treatments to relieve symptoms include lifestyle changes, surgery and medicines to reduce inflammation or suppress the immune system. However, many patients do not respond to medicines and require surgery to repair the damage done to their digestive tract caused during inflammation.
Dr Abigail Raffner Basson, a registered dietitian and scientific researcher at the Digestive Health Research Institute at Case Western Reserve University in the USA, is working to understand the underlying mechanisms causing IBD, and, importantly, how these can be targeted to improve patient outcomes.
A New Mouse Model to Understand the Role of Gut Microbes
Several gut conditions, including IBD, are thought to be affected, if not caused, by abnormal types and amounts of bacteria, and the transfer of gut bacteria from a healthy individual to someone with one of these conditions (a process called faecal microbiota transplant or FMT) is currently being tested as a new treatment option.
Dr Raffner Basson and her team of scientists developed a new mouse model to understand the impact of the human gut microbiome on the development of IBD. They used a type of mouse which has a genetic immunological tendency to develop intestinal disease very similar to Crohn’s disease in humans. These mice can be bred in a germ-free environment which allows the scientists to give them bacteria from people with and without IBD and to see how this affects IBD progression. The team gave gut microbes from nine people, six with IBD in remission and three people who have never been diagnosed with IBD, to these mice and then analysed disease development.
By looking at the bacterial genes in faecal samples, they found that each donor had a distinct microbiota and that the microbiota of the mice closely reflected the donor microbiota. Clear differences in the types of bacteria recovered from donors with IBD and healthy volunteers were seen.
The team then looked at the impact of FMT from different donors on inflammation, indicating IBD in the mice. They found that some donors appeared to cause inflammation, whereas others had no effect or reduced the level of inflammation seen in the mice. Interestingly, this did not seem to correlate with whether the donor had IBD or not – for example, a donor without IBD may or may not induce disease in a mouse. This may explain why FMT from a healthy donor into a patient with IBD is not always effective at reducing disease. If a person is not predisposed to IBD, having low levels of bacteria associated with the disease won’t trigger inflammation for them in the same way it would in a predisposed person. The team then used computational techniques to understand the different metabolic pathways used by the gut bacteria. They found abnormal pathways relating to the metabolism of certain amino acids and fatty acids in the bacteria of IBD patients, which may be an underlying cause of inflammation in this patient group.

The Impact of Diet
Diet is known to play a role in the development of IBD and symptom flare-ups. As well as reducing symptoms and maintaining remission, it is thought that diet affects IBD by impacting the types of bacteria within the gut. Rates of chronic inflammatory conditions such as IBD have been increasing in recent years, potentially due in part to modern Western diets (which are high in animal proteins and refined carbohydrates). Different people will find different foods trigger their IBD symptoms, but in general, red and processed meats, spicy foods, and those high in added sugars and artificial sweeteners have all been associated with increased gut inflammation. Whilst several foods are known to cause inflammation, less is known about anti-inflammatory diets, and there are no specific recommendations for Crohn’s disease patients.
Dr Raffner Basson and her team used the same type of mice, genetically predisposed to developing IBD, to understand which components of our diet influence IBD symptoms. Mice were randomly given either a typical American diet containing animal protein, saturated fat and refined carbohydrates, or a diet where one nutrient was swapped to a ‘healthier’ alternative such as soy-pea protein instead of animal protein or complex carbohydrates instead of refined carbohydrates. The team then analysed the impact of the change in diet on mouse health and gut microbiota.
Mice were fed the different diets for six weeks, and the team found that mice on the soy-pea diet had much less severe inflammation and damage in their guts than the control mice. To test the impact of diet on human IBD bacteria, mice were given the microbiota of a person with IBD or of a healthy volunteer (as validated in their earlier experiments), and then fed the different diets. Remarkably the team observed the same anti-inflammatory effect across all of these groups, with almost no damage to the gut after 24 weeks on the soy-pea diet in comparison to the control mice. The altered fat and carbohydrate diets didn’t have the same impact as the animal to soy-pea protein swap.
The team then used genomic techniques to investigate the types of bacteria present in the mouse digestive tracts. They found that the soy-pea protein diet led to compositional changes, including an increase in lactic acid bacteria which are associated with gut health and nutrient absorption, and a decrease in other species. The team reported these changes in the bacteria demographics within the mouse gut but did not observe a change in the Firmicutes/Bacteroidetes ratio, a common marker of increased IBD risk, suggesting the benefits of the diet are not solely due to the impact on gut bacteria composition. They also found higher levels of healthy amino acids and fatty acids produced by bacteria in the faeces and blood of mice on the soy-pea diet.
Dr Raffner Basson’s work has provided a novel mouse model to help scientists around the world understand the role of the microbiome in the development of IBD as well as a way to test new treatments such as diet. The findings of the group’s study on diet and IBD have important implications, as we now know that replacing animal proteins with soy or pea proteins could reduce levels of inflammation seen in IBD-susceptible people.

The Future of Anti-inflammatory Diets
Due to the team’s remarkable results showing the impact of swapping meat (animal protein) for soy-pea protein in mice, Dr Raffner Basson is currently involved in a human clinical trial to investigate the efficacy of a soy-based diet for Crohn’s disease.
Sixty people made up of those with active Crohn’s disease, Crohn’s disease in remission, and healthy volunteers will fast for 12 hours and then eat a soy-pea-based diet or an identical diet without soy/pea for seven days. After the seven days, Changes to the gut microbiota and the production of key amino and fatty acids will be investigated, along with data collection on patient symptoms, and the number of patients who intend to continue on a high soy diet after the end of the study.
This study is an important milestone for patients with IBD, as whilst there is lots of information available on foods to avoid, there is little knowledge on foods to reduce inflammation and maintain remission. The development of an accessible and noninvasive treatment option offers valuable hope for the many people afflicted with IBD worldwide.
SHARE
DOWNLOAD E-BOOK
REFERENCE
https://doi.org/10.33548/SCIENTIA925
MEET THE RESEARCHER

Dr Abigail Raffner Basson
Department of Nutrition
Division of Gastroenterology & Liver Diseases
Digestive Health Research Institute
Case Western Reserve University
Cleveland, OH
USA
Dr Abigail Raffner Basson is a registered dietitian, National Institutes of Health researcher at Case Western Reserve University, and a clinical dietitian for the Executive Health Center at Cleveland Clinic in the USA. She received her PhD in Public Health and Nutrition from the University of the Western Cape, South Africa. Her work focuses on the underlying mechanisms of inflammatory bowel disease and its treatment through diet, as well as challenging the traditional ‘one size fits all’ approach used in nutrition by underscoring the importance of person-specific host and microbial dietary response. The overarching goal of her work is to translate scientific knowledge and discoveries into applied knowledge that can be disseminated at the community level. Alongside her experience as a clinical dietitian and academic researcher, she has mentored over 100 students both within the hospital and university setting.
CONTACT
W: https://case.edu/medicine/dhri/about/research-team/abigail-basson
KEY COLLABORATORS
Fabio Cominelli, MD, PhD
Division of Gastroenterology and Liver Disease
Digestive Health Research Institute
Case Western Reserve University
Digestive Health Institute
University Hospitals Cleveland Medical Center
Alexander Rodriguez-Palacios, DVM, PhD
Division of Gastroenterology and Liver Disease
Digestive Health Research Institute
Case Western Reserve University
Jeffry Katz, MD
Digestive Health Institute
University Hospitals Cleveland Medical Center
Vu Nguyen, MD
Digestive Health Institute
University Hospitals Cleveland Medical Center
FUNDING
National Institutes of Health (K01 DK 127008-01)
FURTHER READING
AR Basson, A Gomez-Nguyen, P Menghini, et al., Human Gut Microbiome Transplantation in Ileitis Prone Mice: A Tool for the Functional Characterization of the Microbiota in Inflammatory Bowel Disease Patients, Inflammatory Bowel Diseases, 2020, 26, 347–359. DOI: https://doi.org/10.1093/ibd/izz242
A Raffner Basson, A Gomez-Nguyen, A LaSalla, et al., Replacing Animal Protein with Soy-Pea Protein in an “American Diet” Controls Murine Crohn Disease-Like Ileitis Regardless of Firmicutes: Bacteroidetes Ratio, Journal of Nutrition, 2021, 151(3), 579–590. DOI: https://doi.org/10.1093/jn/nxaa386

REPUBLISH OUR ARTICLES
We encourage all formats of sharing and republishing of our articles. Whether you want to host on your website, publication or blog, we welcome this. Find out more
Creative Commons Licence (CC BY 4.0)
This work is licensed under a Creative Commons Attribution 4.0 International License. 
What does this mean?
Share: You can copy and redistribute the material in any medium or format
Adapt: You can change, and build upon the material for any purpose, even commercially.
Credit: You must give appropriate credit, provide a link to the license, and indicate if changes were made.
SUBSCRIBE NOW
Follow Us
MORE ARTICLES YOU MAY LIKE
How Food Environments Shape Our Eating Habits
How we eat dramatically impacts our health, yet millions of Americans live in ‘food deserts’ – areas with limited access to fresh, nutritious food. Recent research reveals that solving this crisis requires looking beyond just physical access to food to understand how our entire community environment shapes our dietary choices. Through a series of pioneering studies, Dr Terrence Thomas and colleagues at North Carolina A&T State University have been investigating how different aspects of our food environment influence what we put on our plates. Their findings suggest that creating lasting change requires reimagining how communities engage with food at every level.
Dr Jim Wu | Ziresovir Offers New Hope for Treating Respiratory Syncytial Virus Infections
Respiratory syncytial virus (RSV) causes respiratory tract infections in children and adults. While for many patients the outcomes of infection are mild, for others, infection can prove fatal, and there is a lack of effective treatments. Dr Jim Wu from the Shanghai Ark Biopharmaceutical Company in China carries out his vital research to develop new, safe, and effective treatments to tackle this killer.
Dr Sandra Grumelli | The Importance of the Choline in Chronic Lung Infections
People with chronic lung conditions like COPD and cystic fibrosis are vulnerable to lung infections caused by the bacterium Pseudomonas aeruginosa. These infections are often difficult to treat and can cause sudden worsening of symptoms, known as flare-ups or acute exacerbations. While we know P. aeruginosa triggers inflammation and damage in the lungs, much less is understood about how exactly it causes these flare-ups, or how it survives in such a harsh environment. Dr Sandra Grumelli from the Center of Investigations of Respiratory Diseases in Argentina, has explored the role of a common molecule called choline which is released during infection. Using a combination of mouse models and laboratory experiments, she has discovered that choline not only makes breathing harder, it also helps P. aeruginosa adapt to and persist in the lungs. Her research opens up new possibilities for tackling chronic infections by targeting the bacteria’s energy use and the way it responds to its environment.
Can Your Personality Shield Your Mind From Ageing? How being open to new experiences might protect against cognitive decline as we age
Many of us have witnessed the troubling effects of ageing on the mind in older friends or family members – the forgotten names, the misplaced keys, the struggle to solve problems that once seemed simple. For decades, scientists have accepted cognitive decline as an inevitable part of growing older. But what if our personality could protect us from some of these changes? A remarkable 25-year study by Dr David Sperbeck, a neuropsychologist at North Star Behavioral Health Hospital in Alaska, has uncovered compelling evidence that certain personality traits might act as a shield against age-related cognitive decline.