Professor Paige Lacy | Deciphering Novel Cytokine Secretion Mechanisms
Following exposure to injury or infection, the body elicits a counteractive immune response which involves many different cell types and processes. Cytokines are substances secreted by cells which play a pivotal role in the regulation of this response. Professor Paige Lacy and colleagues in the Department of Medicine at the University of Alberta in Edmonton, Canada, have conducted extensive research into the exact mechanisms underpinning the regulation of cytokine release during the immune response with a particular focus on airway inflammatory disorders.
Cytokines and the Immune Response
Cytokines are intercellular messengers and purveyors of soluble regulatory signals which mediate the body’s response to injury due to pathogens, allergens and injury. Whilst cytokine release has been extensively studied, the precise mechanisms controlling this process are not yet fully understood, although it is acknowledged that the immune response is multifaceted and involves a complex system of different cell types, transport machinery and molecular pathways.
Over the past two decades, Professor Paige Lacy and her team in the Department of Medicine at the University of Alberta in Edmonton, Canada, have been investigating exactly how cytokines are synthesised, packaged, trafficked and released in response to external stimuli which cause cellular damage. Their work has identified many enzymes, membrane proteins, and receptors involved in these processes, and has revealed novel mechanisms of action in the regulation of the immune response in allergic airway inflammation and asthma.
Initially, Professor Lacy and colleagues reviewed published evidence to identify knowledge gaps relating to the mechanisms of cytokine release from immune cells. They explained that cytokine secretion by a range of cell types is a fundamental aspect of the immune response, and greatly influences the body’s reaction to stimuli.
Credit Paige Lacy
Cytokine Secretion Pathways
Many different cells secrete cytokines, including epithelial cells, eosinophils, and macrophages. Epithelial cells are omnipresent, forming thin layers of lining tissue throughout the body, and are among the first cells to release cytokines in response to harmful signals. Epithelial cells work closely with the immune system by sending cues to initiate appropriate physiological reactions. Innate immune cells, such as macrophages and eosinophils, are naturally occurring cells which rapidly mobilise to the site of injury or infection, and can generate a wide range of cytokines. Collectively, these cells control pathogen invasion by recognising threats and producing toxic substances which kill harmful invaders, although the mechanisms relating to the movement of cytokines from epithelial cells prior to release remain to be fully determined.
Cytokines may be secreted via classical or non-classical pathways, which are defined depending upon the specific mode of action, and several pathways have been identified in specific immune cells. A major purpose of each pathway is to selectively regulate temporal cytokine release and to suitably terminate the response when necessary.
Most cytokine secretion, including from eosinophils, is via the classical pathway which is characterised by the packing and storage of cytokines in secretory granules within the cell prior to receptor-induced regulated release facilitated by membrane fusion. Alternatively, such as in macrophages, cytokines may be released immediately following synthesis which can ensue in a polarised manner. Furthermore, the process of cytokine secretion is customisable depending upon the required cell-specific immune function.
Eosinophils are highly granulated white blood cells which increase in abundance during an allergic response, and are capable of synthesising, storing, and secreting up to 35 different cytokines. Eosinophils have been observed in the airways of around half of asthma sufferers and may contribute to tissue damage. Cytokine secretion from eosinophils occurs predominantly via so-called piecemeal degranulation, where cytokines are recruited from larger storage granules and transported to the cell membrane in smaller vesicles, and degranulation may also occur via classical or compound exocytosis, as well as by lysis in dying cells.
Macrophages are derived from white blood cells predominantly found on mucosal surfaces including the airways and have a key role in wound healing and tissue repair. Cytokines within macrophages are continuously transported to the cell surface in preparation for release when these cells are activated.
Professor Lacy and her team summarised that the movement of cytokines through immune cells is dependent upon membrane-bound or cytoplasmic enzymes, proteins, trafficking molecules, and intracellular membrane receptors, which mediate transport, facilitate membrane fusion, and regulate secretion. Initiation of the secretion pathway occurs within minutes of encountering an agonist. However, the specific roles of certain enzymes and proteins and the importance of cellular structural rearrangements in cytokine release from innate immune cells had not yet been elucidated.
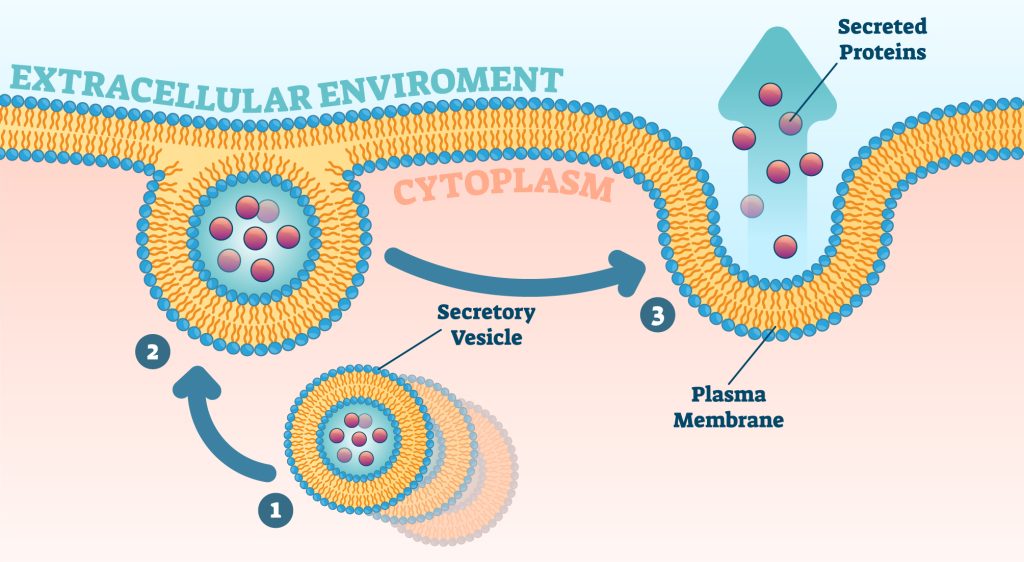
Illustration of cytokine secretion
Determining Cytokine Secretion Mechanisms
Given the paucity of available information, Professor Lacy and colleagues attempted to determine which molecules regulate eosinophil degranulation within the context of airway inflammation. To do this, the team built upon an earlier study in which they discovered that asthma patients exhibited a higher expression and activity of a specific enzyme (Rab27a) within their eosinophils, and that this likely contributed to the physiological traits typically observed in asthma. Human and mouse eosinophils were isolated and subjected to various laboratory techniques to determine the presence, subcellular localisation, and polarisation of the selected molecule.
They found that the molecule selectively redistributed when the cells were stimulated with an agonist, which suggested that eosinophil cytokine release indeed occurred in a manner that was dependent on Rab27a. Further studies in eosinophils demonstrated a role for other intracellular enzymes and receptor proteins (Cdk5, VAMP-7). Professor Lacy and her team confirmed these findings by repeating the experiments in strains of mice which had been genetically modified to eliminate the proteins necessary for normal eosinophil function and observed that degranulation responses became defective. This research identified for the first time a direct role for specific regulatory molecules in inducing and controlling eosinophil degranulation in allergic inflammation and asthma.
Following these encouraging insights, Professor Lacy and her team endeavoured to further classify the proteins involved in the degranulation of eosinophils, since stimuli-induced activation of eosinophils is recognised as an exacerbating factor in the airway hyperresponsiveness associated with asthma. The researchers selected a vesicle-associated membrane protein (VAMP-7) which had previously been identified as an essential component of degranulation and confirmed that it was present in mouse eosinophils using fluorescence microscopy. Upon stimulation, isolated eosinophils translocate to gather at the edge of the cell, preparing for the release of granular contents.
Furthermore, genetically modified mice models lacking the chosen protein and mimicking allergic airway inflammation demonstrated a reduced incidence of degranulation and fewer cell-damaging products being released, suggesting a dysfunction in the eosinophil activation process, and confirming that eosinophil degranulation contributes to airway hyperresponsiveness. The fact that degranulation was not entirely abolished may be attributed to the small proportion of eosinophils that release their granular contents upon cell lysis, a recognised occurrence in allergic responses which depends on different signalling mechanisms. The researchers concluded that airway inflammation is at least partly mediated by degranulating eosinophils which can directly exacerbate the condition.
A Role for Cellular Structural Changes
To further investigate the mechanisms of cytokine secretion, Professor Lacy and colleagues proceeded to evaluate the intracellular storage sites of selected cytokines in eosinophils, and the pathways involved in their release. First, the team isolated human eosinophils from allergic or asthmatic participants and stimulated them to initiate cytokine trafficking. Fluorescence microscopy revealed altered eosinophil morphology and spatiotemporal increases in the levels of some cytokines following stimulation. Thereafter, the team deduced that membrane recycling pathways are likely employed by eosinophils to transport certain cytokines to the cell membrane for release, providing further insight into trafficking mechanisms within eosinophils.
This finding echoed that of earlier research conducted by Professor Lacy and her team investigating the mechanisms of cytokine secretion in macrophages, during which they reported that newly synthesised cytokines were also trafficked via a membrane recycling pathway. Delving further, the team continued to explore the mechanisms underlying the trafficking pathways and establish which mediators may be involved in the associated cellular structural changes. Using fluorescence microscopy techniques, dramatic alterations in the shape of cells were observed in the presence of a specific enzyme (Rac1), which was also associated with increased release of a selected cytokine and found to be vital for the final trafficking step prior to secretion within activated macrophages. Indeed, inhibition of the selected enzyme did not prevent cytokine synthesis in macrophages but did reduce transport and secretion, thus confirming, for the first time, its essential role in cytokine trafficking via the membrane recycling pathway.
Implications for Future Study
Understanding the various intercellular pathways involved in cytokine secretion is crucial for increasing our knowledge of cellular function in innate immunity and the associated ramifications for disease. Further studies surrounding the interrelationships of the regulatory pathways involved in the transport and secretion of cytokines and pro-inflammatory mediators may help to determine the underlying mechanisms unique to individual cell types. This is particularly prudent in the study of the mechanisms of cytokine release via non-classical pathways, since the theories surrounding this remain controversial.
More in-depth research to assess the secretion pathways of a wider range of cytokines and different cell types will undoubtedly prove highly beneficial in elucidating the underlying mechanisms of these phenomena. Using increasingly refined models of disease states has enabled Professor Lacy, her team, and collaborators to elicit the role of specific proteins in the degranulation of eosinophils in allergic inflammation using sophisticated gene targeting strategies. It is probable that complex multimodal mechanisms are involved in airway hyperresponsiveness involving synergistic product relationships, and experiments to decipher the contribution of individual components of eosinophil degranulation in asthmatic inflammation are warranted.
Perhaps most encouragingly, there is scope for exciting collaborations between scientific and clinical teams to apply the knowledge gained regarding the mechanisms of cytokine release in inflammatory disorders to the development of novel therapeutic targets.
SHARE
DOWNLOAD E-BOOK
LISTEN TO THE AUDIO
REFERENCE
https://doi.org/10.33548/SCIENTIA843
MEET THE RESEARCHER

Professor Paige Lacy
Department of Medicine
University of Alberta
Edmonton
Canada
Professor Paige Lacy received her PhD in cell physiology from Wellington School of Medicine at the University of Otago, New Zealand. Following her inaugural postdoctoral fellowship, Professor Lacy held several assistant professor roles before attaining full professorship in her current role at the University of Alberta. The primary focus of Professor Lacy’s research is to elucidate the molecular and cellular mechanisms involved in inflammatory responses, and in particular, the release of cytokines by innate immune cells. In addition to her plethora of accolades, Professor Lacy has led several research groups and education programmes in her capacity as former director of Alberta Respiratory Centre and has been the recipient of many coveted awards in recognition of her outstanding contributions to allergy research. Professor Lacy is a member of the prestigious Collegium Internationale Allergologicum, as well as numerous professional societies, and has published more than 126 peer-reviewed articles to date.
CONTACT
E: placy@ualberta.ca
W: https://www.ualberta.ca/medicine/about/people/details.html?n=paige-lacy
Twitter: @UAProfessor
KEY COLLABORATORS
Dr Jamie Lee, Mayo Clinic Scottsdale
Dr Manali Mukherjee, McMaster University
Dr Parameswaran Nair, McMaster University
Dr Helene Rosenberg, National Institutes of Health
Dr Jennifer L. Stow, Institute for Molecular Bioscience, University of Queensland
FUNDING
Alberta Heritage Foundation for Medical Research
Australian Research Council International Discovery Grant
Canadian Institutes of Health Research
National Health and Medical Research Council of Australia
Natural Sciences and Engineering Research Council of Canada Discovery Grant
FURTHER READING
S Almas, O Srivastava, N Fayad, et al., Cytokine trafficking of interleukin-9 and interleukin-13 through TfnRc+ vesicles in activated human eosinophils, Journal of Leukocyte Biology, 2021, 94, 1265–1274. DOI: https://doi.org/10.1002/JLB.2MA0820-320RR
L Willetts, LC Felix, EA Jacobsen, et al., Vesicle-associated membrane protein 7-mediated eosinophil degranulation promotes allergic airway inflammation in mice, Communications Biology, 2018, 1, 83, DOI: https://doi.org/10.1038/s42003-018-0081-z
AC Stanley, CX Wong, M Micaroni, et al., The Rho GTPase Rac1 is required for recycling endosome-mediated secretion of TNF in macrophages, Immunology and Cell Biology, 2014, 92, 275–286. DOI: https://doi.org/10.1038/icb.2013.90
JD Kim, L Willetts, S Ochkur, et al., An essential role for Rab27a GTPase in eosinophil exocytosis, Journal of Leukocyte Biology, 2013, 94, 1265–1274. DOI: https://doi.org/10.1189/jlb.0812431
P Lacy, JL Stow, Cytokine release from innate immune cells: association with diverse membrane trafficking pathways, Blood, 2011, 118, 9–18. DOI: https://doi.org/10.1182/blood-2010-08-265892
AC Stanley, P Lacy, Pathways for cytokine secretion, Physiology (Bethesda), 2010, 25, 218–229. DOI: https://doi.org/10.1152/physiol.00017.2010

REPUBLISH OUR ARTICLES
We encourage all formats of sharing and republishing of our articles. Whether you want to host on your website, publication or blog, we welcome this. Find out more
Creative Commons Licence (CC BY 4.0)
This work is licensed under a Creative Commons Attribution 4.0 International License. 
What does this mean?
Share: You can copy and redistribute the material in any medium or format
Adapt: You can change, and build upon the material for any purpose, even commercially.
Credit: You must give appropriate credit, provide a link to the license, and indicate if changes were made.
SUBSCRIBE NOW
Follow Us
MORE ARTICLES YOU MAY LIKE
Dr JoLee Sasakamoose – Dr Mamata Pandey | Empowering Indigenous Health: The Indigenous Wellness Research Collaborative in Saskatchewan
The Indigenous Wellness Research Collaborative is a transformative alliance dedicated to advancing health systems and service delivery for Indigenous communities across Saskatchewan. Founded a decade ago and co-led by Dr Mamata Pandey, a research scientist at the Saskatchewan Health Authority, and Dr JoLee Sasakamoose (M’Chigeeng First Nation), Canadian Institute of Health Research Chair in Indigenous Wellness and Health Equity at the University of Regina, their team’s work is rooted in a commitment to Indigenous leadership and community-defined wellness goals. Guided by the Cultural Responsiveness Framework, the Collaborative prioritises creating ethical spaces that serve as a middle ground for respect, reciprocity, and authentic partnerships. The team employs a strengths-based approach to health research, centering Indigenous methodologies that respect the interconnectedness of spiritual, mental, emotional, and physical well-being.
Professor Jaya Krishnan | Revolutionary Gene Therapy Helps Hearts Regenerate After Heart Attacks
Myocardial infarction, commonly termed as a heart attack, is a major cause of death and poor health worldwide. Regenerating heart tissue is an exciting and promising concept that can have significant benefits in myocardial infarctions and related diseases, but this has not yet been achieved in real-life clinical treatments. In a collaboration between Goethe University Frankfurt and Goethe University Hospital, Professor Jaya Krishnan and colleagues address this by controlling pathologic genes involved in the development of heart failure that develops after heart attacks. The researchers demonstrate a new way of treating heart disease by aiding in the division and regrowth of heart cells after a heart attack.
James J. Driscoll, MD, PhD | Immunoproteasome Activation Enhances the Recognition of Tumour Cells and Boosts Anticancer Immune Responses
The correct functioning of the human immune system depends on its ability to recognise danger, such as tumour cells, viruses, and bacteria. Scientists are learning how immunoproteasome activation can overcome the mechanisms by which cancer cells escape immune responses. Immunoproteasomes are small high molecular weight protein-degrading machines that signpost abnormal proteins made by cancer cells, directing the immune system against them. Dr James Driscoll at University Hospitals Cleveland Medical Center is using novel proprietary small molecules to selectively boost the catalytic activity of immunoproteasomes, which increases the tumour killing (or cytotoxic) effect of a group of white cells called T-cells. These findings provide a strong rationale for developing personalised therapeutics that target immunoproteasomes, for cancer and other immune-mediated conditions.
New Approaches to Treating Alzheimer’s Disease
Alzheimer’s disease is a devastating condition that strips away people’s memory, thinking, and independence. By 2050, it is expected to affect over 100 million people around the world, making it a high priority for scientific and medical research. Researchers are now exploring the potential for mechanical and light-based stimulation of the brain and nervous system to treat Alzheimer’s disease symptoms. At the University of Minho in Portugal, Francisca Monteiro is developing a PhD project supervised by a multidisciplinary set of experienced researchers, who have reviewed the evidence behind these approaches, including whole-body vibration, auditory stimulation, transcranial ultrasound stimulation, and photobiomodulation. The team aims to synthesize the evidence to support these treatments and understand what further work is needed.