Dr Alyson J McGregor | Uncovering the Gender Gap in Medical Research: How Sex Differences Impact Healthcare Outcomes
Medical research has historically focused predominantly on male subjects, leading to dangerous gaps in our understanding of how diseases and treatments affect women. Dr Alyson McGregor from University of South Carolina School of Medicine Greenville has devoted her career to addressing this critical issue, highlighting how biological sex differences impact health outcomes. Her work demonstrates that ignoring these differences can have life-threatening consequences and advocates for more inclusive research practices to ensure safe and effective healthcare for everyone.
The Invisible Woman in Medical Research
Until recently, women have been largely excluded from clinical trials and medical research. This exclusion was often justified by concerns about fluctuating hormone levels affecting results or potential risks to reproductive health. However, this male-centric approach has created a significant blind spot in medical knowledge, with treatments tested primarily on men being routinely prescribed to women without understanding how biological sex differences might affect outcomes.
The consequences of this oversight can be devastating. According to a 2001 US Government Accountability Office report, eight out of ten drugs withdrawn from the market between 1997 and 2000 posed greater health risks for women than for men. These withdrawn medications had caused serious adverse reactions in women, including fatal arrhythmias, valvular heart disease, and liver failure – side effects that might have been identified earlier if women had been properly included in clinical trials.
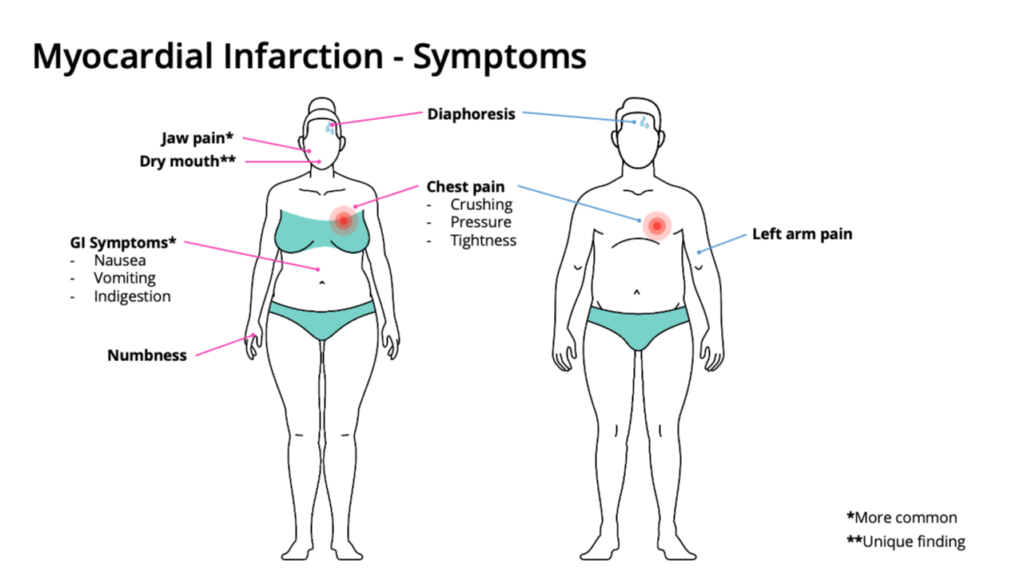
Even when women experience common medical conditions, their symptoms may differ significantly from textbook descriptions based on male patients. Heart attacks provide a classic example: while men typically experience crushing chest pain radiating down the left arm, women often present with subtler symptoms like fatigue, shortness of breath, or discomfort in the jaw, neck, or back. These ‘atypical’ presentations – atypical only because they differ from the male standard – can lead to delayed diagnosis and treatment.
This bias extends to medical education as well. Medical students learn from textbooks that often use male figures as the default anatomical models, with female structures presented as ‘add-ons’. The electronic medical records used in hospitals frequently display male thorax images, even when documenting female patients with chest or abdominal pain. This reinforces the notion that male bodies represent the ‘norm’ in medicine, while female bodies are variations requiring special consideration.
The Impact of Gender in Healthcare
Dr Alyson McGregor, an emergency medicine physician and researcher at the University of South Carolina School of Medicine Greenville has been at the forefront of efforts to address these disparities. She emphasises that both biological sex (the chromosomal, hormonal, and anatomical characteristics) and sociocultural gender (the roles, behaviours, and identities constructed by society) influence health outcomes.
Dr McGregor explains that women’s biology differs from men’s in ways that affect how medications are processed in the body. Women tend to have different body weights, body fat percentages, plasma volumes, and organ blood flow – all factors that impact drug absorption and distribution. Additionally, the liver shows more than 1,000 genes with sex-specific expression patterns, altering how drugs are metabolised. Many medications, including common ones like paracetamol, benzodiazepines, and propranolol, are cleared by the kidneys at different rates in women compared to men.
Hormone fluctuations during the menstrual cycle further complicate matters. For example, Dr McGregor points out that antiplatelet therapies show different effectiveness depending on hormonal status, and antiepileptic medications can become subtherapeutic during certain phases of the menstrual cycle, potentially triggering seizures that could have been prevented with appropriate dosage adjustments.
Recognising the Problem
The good news is that awareness of these issues is growing. In a review published in the Journal of Women’s Health, Dr McGregor and colleagues analysed the impact of Food and Drug Administration (FDA) guidelines implemented after the 2001 GAO report. Their findings indicate that changes to promote drug safety for women have had measurable effects, with a 67% reduction in yearly post-market drug withdrawals due to unanticipated adverse reactions in women.
Key policy changes included the Demographic Rule, which requires representation of both sexes in drug trials, and the FDASIA Section 907 Action Plan calling for sex-disaggregated data analysis. The FDA also provided official guidance for monitoring drugs’ effects on cardiac arrhythmias and liver failure, particularly in women.
Despite these advances, Dr McGregor emphasises that significant gaps remain. Current regulations do not specify what percentage of women must be included in clinical trials, meaning that technically any level of female participation, however minimal, could satisfy requirements. In some cases, this loophole allows for troubling exclusions. For instance, as recently as 2019, the FDA approved an HIV prevention drug combination for men and transgender women without requiring testing in cisgender women.
From Invisibility to Leadership
In addition to addressing research disparities, Dr McGregor highlights another critical issue: the underrepresentation of women in academic medicine leadership positions. While women now represent 51.6% of medical school students and over half the healthcare workforce, they remain significantly underrepresented at the highest levels of medical academia and leadership.
Dr McGregor argues that this gender inequity is not merely a workplace issue but has broader implications for medical research and patient care. Studies have shown that the presence of women in research teams, especially as first and last authors, increases the likelihood of appropriate sex- and gender-based analyses in published papers. After reviewing more than 1.5 million research articles, researchers found that women comprised 40% of first authors, 27% of last authors, and 35% of authors overall in disease-specific research — numbers that suggest progress but also indicate continued disparities.
The barriers women face in academic medicine include explicit and implicit bias, unequal division of domestic responsibilities, lack of effective mentorship, and institutional cultures that inadvertently disadvantage women. These challenges can lead to women being passed over for promotion and leadership opportunities, slowing career advancement and reducing their influence in the field.
Impact on Patient Care
The consequences of these research and leadership gaps extend beyond academic concerns to directly affect patient care. When medical decisions are based on research conducted primarily on men, both male and female patients may receive suboptimal treatment.
Dr McGregor points to the example of zolpidem (Ambien), a widely prescribed sleep medication. It took the FDA 21 years after initial approval to recognise that the original dosing was dangerous for women, ultimately leading to new requirements in 2013 that reduced the maximum dose for women by 50%. This delay potentially exposed millions of women to excessive doses and unnecessary side effects.
Similarly, heart disease, the leading cause of death for women in many countries, often presents differently in women than in men. Because medical education has traditionally focused on male-pattern symptoms, healthcare providers may miss or delay diagnosis in female patients, leading to worse outcomes.
Moving Toward Gender Equity
Dr McGregor advocates for a comprehensive approach to addressing gender disparities in medicine. She recommends incorporating sex and gender differences into medical education, ensuring that future healthcare providers understand how these factors influence disease presentation, diagnosis, and treatment. Additionally, she calls for strengthening research requirements to ensure meaningful inclusion of women in clinical trials and appropriate sex-disaggregated data analysis.
The researcher also emphasises the importance of supporting women’s advancement in academic medicine through mentorship, policy changes, and institutional support. Promoting awareness of gender bias among all healthcare providers and researchers, while engaging men as allies in addressing gender inequities, forms another crucial aspect of her approach.
Dr McGregor emphasises that these changes will benefit all patients, not just women. By developing a more nuanced understanding of how sex and gender affect health, medical research can produce treatments that are safer and more effective for everyone.
The Power of Education and Awareness
Education plays a pivotal role in addressing gender disparities in medicine — for both patients and healthcare providers. Dr. McGregor is a passionate advocate for embedding sex- and gender-based medical concepts into healthcare education and equipping patients with science-backed information to advocate for their own health.
To bring this vision to life, Dr. McGregor co-founded the OM Health Hub, a comprehensive platform that creates health programs in collaboration with experts who understand how sex and gender influence health outcomes. The platform employs an innovative educational model that combines scientific rigor with engaging content to reach a broad audience, including clinicians, patients, and the general public.
By making this knowledge widely accessible, Dr. McGregor seeks to accelerate the integration of sex- and gender-informed approaches into mainstream medical practice. She argues that education is essential not only for addressing implicit bias, but also for ensuring that care is tailored to the diverse biological and social realities of all patients.
Looking Forward to a More Equitable Future
Dr McGregor’s work highlights both the challenges and opportunities in addressing gender disparities in medicine. While significant progress has been made, particularly in regulatory requirements for drug testing, much work remains to be done to ensure genuine equity in research, education, and clinical practice.
The path forward requires continued advocacy, policy changes, and cultural shifts within medical institutions. It also depends on recognising that addressing gender inequities is not a special interest issue but a fundamental aspect of providing high-quality, evidence-based healthcare.
In her publications, Dr McGregor consistently emphasises that women and men in medicine must collaborate to support, educate, and promote each other. She believes our mission as healers of patients and teachers of future generations of healers requires embracing the true perspective of equality to guide the way forward.
By highlighting the importance of sex and gender differences in health and advocating for more inclusive research and practice, Dr McGregor’s work points toward a future where medicine truly serves all patients equally — a goal that benefits everyone, regardless of sex or gender.
SHARE
DOWNLOAD E-BOOK
REFERENCE
https://doi.org/10.33548/SCIENTIA1277
MEET THE RESEARCHER

Dr Alyson J McGregor
Associate Dean of Faculty Affairs and Development, University of South Carolina School of Medicine Greenville, South Carolina, USA
Dr Alyson McGregor is a Professor of Emergency Medicine and Associate Dean of Faculty Affairs and Development at the University of South Carolina School of Medicine Greenville. She received her Doctor of Medicine from Boston University School of Medicine in 2003 and completed her Emergency Medicine Residency at Rhode Island Hospital through Brown University (2003–2007). Dr McGregor is a pioneering researcher and advocate for sex and gender-based medicine, having founded and directed the Division of Sex and Gender in Emergency Medicine at Brown University (2010–2021). She received an Honorary Doctorate of Science from the University of New Hampshire in 2023 and is a Fellow of the American College of Emergency Physicians. Dr McGregor is an internationally recognised expert who has authored numerous publications, including two influential books, Sex Matters: How Male Centric Medicine Endangers Women’s Health and What We Can Do About It, and Why Women Aren’t Winning at Health (but can).
CONTACT
E: Alyson.McGregor@prismahealth.org
W https://sc.edu/study/colleges_schools/medicine_greenville/about/deans_admin/mcgregor.php
X: https://www.alysonmcgregormd.com
https://www.linkedin.com/in/alyson-j-mcgregor-77433845/
https://www.instagram.com/amcgregormd/
KEY COLLABORATORS
Dr. Marjorie Jenkins, University of North Dakota (UND), Vice President for Health Affairs and Dean of UND Medical School
Anca Griffith, CEO at OM Health Hub
American Medical Women’s Association
Women’s Health Access Matters
FUNDING
National Institutes of Health Office of Research on Women’s Health
Society for Academic Emergency Medicine
Brown Physicians Inc.
Society of Family Planning Research Fund
FURTHER READING
AJ McGregor and B Becker, Food and Drug Administration Advances Drug Safety for Women: First Steps in a Long Journey, Journal of Women’s Health, 2021, 00 (00). DOI: https://doi.org/10.1089/jwh.2020.8962
AJ McGregor, Gender Inequity in Academic Medicine: A Visible Sign of a Disseminated Disease, Journal of Women’s Health, 2020, 29, 2. DOI: https://doi.org/10.1089/jwh.2019.8152
AJ McGregor, G Beauchamp, and C Wira, et al., Sex as a Biological Variable in Emergency Medicine Research and Clinical Practice: A Brief Narrative Review, Western Journal of Emergency Medicine, 2017, 18, 6, 1077–1088. DOI: https://doi.org/10.5811/westjem.2017.8.34997

REPUBLISH OUR ARTICLES
We encourage all formats of sharing and republishing of our articles. Whether you want to host on your website, publication or blog, we welcome this. Find out more
Creative Commons Licence (CC BY 4.0)
This work is licensed under a Creative Commons Attribution 4.0 International License. 
What does this mean?
Share: You can copy and redistribute the material in any medium or format
Adapt: You can change, and build upon the material for any purpose, even commercially.
Credit: You must give appropriate credit, provide a link to the license, and indicate if changes were made.
SUBSCRIBE NOW
Follow Us
MORE ARTICLES YOU MAY LIKE
Dr Hatim Hassan | Proteins identified in gut bacteria that reduce oxalate levels
New research has identified proteins from gut bacteria, called Sel1-like proteins, that have the potential to help the body get rid of excess oxalate, an organic substance linked to kidney stones, kidney disease, and other health problems. Sel1-like proteins help the cell in assembling large molecular complexes important for cell function. Dr Hatim Hassan from the Division of Nephrology and Hypertension, Mayo Clinic, Rochester, Minnesota, United States, is part of a team of scientists researching whether these proteins and their derived peptides could reduce blood and urinary oxalate levels to prevent and/ or treat hyperoxalemia (high blood oxalate), hyperoxaluria (high urine oxalate) and related disorders (including kidney stones).
Dr Norio Mitsuhashi | Measuring Respiratory Motion to Improve Precision in Lung Radiation Therapy
Dr Norio Mitsuhashi, former Professor of the Department of Radiation Oncology at Tokyo Women’s Medical University, leads revolutionary clinical research into optimising stereotactic body radiation therapy for lung cancer. Dr Mitsuhashi and his colleagues examine whether routinely available patient and tumour characteristics can predict respiratory tumour motion, a critical source of uncertainty in high precision radiotherapy. Their findings suggest that respiratory motion cannot be reliably inferred, and must instead be measured directly in every patient.
Professor Terry C. Hrubec | Clean is good – but is too clean better?
Quaternary ammonium compounds are a large class of compounds used as disinfectants in hospitals, restaurants, healthcare and animal care facilities, and are popular as household cleaners. With disease outbreaks increasing our fears about infections, the use of disinfectants has skyrocketed in recent years. Understandably, we all want to feel safe. However, as Professor Terry Hrubec from the Department of Biomedical Sciences of E. Via College of Osteopathic Medicine discovered, such products may be causing more harm than good.
Professor Richard Ludueña | Two Turkish Cities Were Essential in the Development of Science and Religion – a Work in Progress
This book explores the history of the area in Turkey where these two cities lie. Prof Richard Ludueña and his daughter visited Harran and Sanliurfa (formerly Edessa) in 2014. He found them fascinating and wanted to learn more about their histories, but found no book that focused on their history from the beginning to modern times. So, he decided to write one.
Harran still bears its ancient name, but Edessa has had a great variety of names and is now called Sanliurfa. Our story goes back long before the cities were founded, back to the late Neolithic site of Göbekli Tepe, where monuments have carvings consistent with a destructive comet.