Dr. Erin Norris – Novel Biomarkers and Promising Therapeutic Targets in Alzheimer’s Disease
Alzheimer’s disease is a form of dementia that affects tens of millions of people globally. Although we can modestly improve the quality of life of patients, there is currently no cure, largely because the underlying biological mechanisms of the disease are poorly defined. Understanding the abnormal molecular characteristics of Alzheimer’s disease is the focus of Dr. Erin Norris’s research at The Rockefeller University. By studying the dysfunction of the plasma contact system, which may result in abnormal coagulation and inflammation that may lead to Alzheimer’s disease, Dr. Norris and her colleagues have uncovered novel biomarkers, paving the way for exciting new therapeutics.
A Common but Challenging Disease
Alzheimer’s disease is the most common form of dementia, which is an umbrella term encompassing a variety of diseases characterised by a progressive decline in cognitive functions such as memory, language, attention and reasoning. The symptoms often initially present as minor problems with memory that progress into confusion, issues with speech and movement, alterations in personality like aggression, and even hallucinations. Risk factors for Alzheimer’s disease include a family history of the condition, older age, lifestyle factors associated with cardiovascular disease and untreated depression.
While people do not tend to pass away from the illness itself, many patients experience a reduced appetite and their diminished cognitive ability can result in difficulty swallowing, causing inhalation of food and frequent chest infections. Currently, there is no cure but certain drugs can alleviate some of the symptoms. Psychological treatments such as cognitive stimulation therapy can try to help prevent the further deterioration of memory and language. Changing the home environment in which a person with Alzheimer’s disease resides can also allow them to live more independently by simplifying day-to-day tasks.
Research across the globe has been dedicated to finding and targeting the molecular irregularities that cause Alzheimer’s disease. Although the exact causes are not well-defined, it is understood that when proteins (the building blocks of all cells) in the brain act abnormally, the function of brain cells known as neurons is disrupted. The subsequent series of toxic events results in damage to neurons. The connections that facilitate brain activity are also disrupted, which eventually causes the neurons to die, leading to a decline in cognitive function.
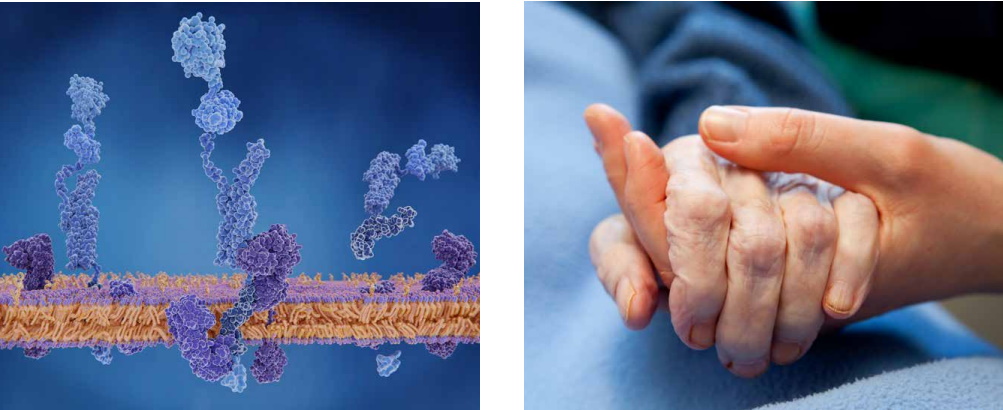
The proteins responsible for these destructive events are called beta-amyloid and tau. Beta-amyloid is a fragment of a very large protein called amyloid precursor protein. When these fragments aggregate they disrupt cell-to-cell communication and continue to cluster with other cellular debris into large deposits called amyloid plaques. These plaques can then also lead to chronic inflammation in the brain, which is toxic to neurons. Tau proteins are important for the internal support of neurons and help to carry essential nutrients and materials. However, in Alzheimer’s disease, tau proteins become atypically organised to create neurofibrillary tangles which disrupt the transport system.

Targeting the Plasma Contact System
These pathologies of Alzheimer’s disease have been extensively studied, but an issue that has been less explored is vascular dysfunction – problems in blood vessels and blood circulation. Many patients experience a reduced blood flow in the brain known as hypoperfusion, damage to brain blood vessels and disruption to normal mechanisms that stop bleeding and repair damage (haemostasis). Vascular disorders such as obesity, hypertension and diabetes are also common in those with Alzheimer’s. Dr. Erin Norris and her colleagues from The Rockefeller University in New York are working to understand the links between Alzheimer’s and vascular dysfunction and the biological processes behind them.
The vascular system is responsible for coagulation, which is the process of liquid blood changing into a solid state, or blood clot, to repair injuries. There are two mechanisms by which this occurs – the first is extrinsic clotting. When an injury or trauma occurs outside of the blood vessel (a cut, for example), this pathway is activated to heal the damage. The other is intrinsic clotting, which occurs when there is trauma to the blood vessel itself or the tissues surrounding it. These two mechanisms merge together to form blood clots via the cleavage (cutting up) of fibrinogen proteins into smaller fibrin proteins using an enzyme called thrombin.
Research from Dr. Norris and her scientific team has revealed that the intrinsic clotting pathway in patients with Alzheimer’s is disrupted, whilst the extrinsic system is left intact. In one study, Dr. Norris and her colleagues investigated the plasma contact system within the intrinsic pathway. This system is initiated by a protein called coagulation factor XII (FXII) being activated into its active form (FXIIa), which then triggers two arms of the process. One arm is the clotting pathway that utilises factor XI (FXI) to produce thrombin and blood clots, while the other is an inflammatory pathway that uses prekallikrein (PK) to produce the pro-inflammatory peptide, bradykinin.
Bradykinin is cleaved out of high molecular weight kininogen (HK) by the activated form of PK (or PKa). HK is important for both arms of the system because it forms complexes with both FXI and PK allowing for their efficient activation by FXIIa. Due to this dual function of HK, reducing or inhibiting the cleavage of HK can prevent unwanted blood clots and inflammation, as shown in some of Dr. Norris’s experiments. To prevent HK cleavage, they depleted the amount of FXII in Alzheimer’s model mice, which in turn prevented the function of HK. The mice showed reduced neuroinflammation and neurodegeneration and performed better cognitively compared to untreated mice.
These exciting results demonstrate a potential novel focus for Alzheimer’s therapies. As contact system activation may play a part in the pathology of Alzheimer’s, blocking it could slow disease progression. Dr. Norris suggests HK as a prime target in the quest to prevent inflammation as well as abnormal coagulation, and her team has already discovered a way of inhibiting the protein’s cleavage. Her method utilises an antibody that binds to HK and prevents its cleavage and thus its ability to generate bradykinin. Whilst the antibody is being tested, she studies other abnormal molecular occurrences in Alzheimer’s patients.
Defining Biomarkers for Alzheimer’s Disease
The overactivation of the intrinsic pathway in Alzheimer’s could be due to the unusual build-up of beta-amyloid protein. Beta-amyloid can bind to FXII and lead to activation of the plasma contact system, resulting in a high amount of cleaved HK and bradykinin in the plasma of Alzheimer’s patients as well as mouse models. While not all Alzheimer’s patients have vascular dysfunction and contact system activation, being able to identify those patients suffering from this condition would be advantageous as there are already FDA-approved treatments. Any method to slow the progression of the disease in even a subset of patients would be beneficial. Therefore, cleaved HK could be categorised as a biomarker, and could be a useful means of diagnosing Alzheimer’s patients with vascular dysfunction.
In order to create a diagnostic tool, Dr. Norris’s laboratory team set out to generate and screen for antibodies that could specifically recognise both the cleaved and uncleaved versions of HK. Once these were identified, they used a method called enzyme-linked immunosorbent assay to screen for these proteins in human plasma. The tests revealed decreased uncleaved HK and increased cleaved HK in those plasma samples from Alzheimer’s patients, and these results correlated with dementia and levels of beta-amyloid plaque in the brain. This study provides solid evidence that cleaved HK in plasma could be used as a novel biomarker for the diagnosis of Alzheimer’s disease with a vascular pathophysiological component.
Dr. Norris continued to explore this avenue in a subsequent study that centred around mild cognitive impairment (MCI). This disorder is a transitional stage between the normal cognitive decline that comes with ageing and the commencement of mild dementia. Patients with MCI tend to adequately carry out daily tasks but have some deficits in cognitive function such as short-term memory retrieval. Approximately 10–15% of MCI patients convert to an Alzheimer’s diagnosis per year.
Dr. Norris’s team examined the plasma of MCI patients for evidence of contact system activation. Aligning with their previous results, those living with MCI who experienced poor memory recall had increased kallikrein activity and subsequently, higher levels of cleaved HK. This finding further supported her and her team’s hypothesis that contact system dysfunction is a biomarker for Alzheimer’s and its related dementias as it can contribute to its pathogenesis.
Implementing Novel Biomarkers
A further study by Dr. Norris’ group showed significantly elevated levels of bradykinin in the plasma of Alzheimer’s patients compared to healthy participants. Increased levels of bradykinin are due to increased contact system activation and cleavage of HK. Furthermore, those with a more profound increase in bradykinin displayed more severe cognitive impairment. These results strongly suggest that cleaved HK and bradykinin are involved in disease pathogenesis. Moreover, since bradykinin is a potent inflammatory molecule, it could be responsible for much of the neuroinflammation found in Alzheimer’s patients. Interestingly, post-mortem examination of Alzheimer’s patients’ brain tissue showed that bradykinin co-deposits with beta-amyloid plaques.
Dr. Norris and her colleagues at The Rockefeller University have uncovered multiple, yet linked, biomarkers for Alzheimer’s disease, and they are continuing their research into how they can be targeted to develop novel and effective therapeutics. They are particularly focused on an anti-HK antibody called 3E8 which binds very strongly to HK to inhibit the activation of the contact system by beta-amyloid to prevent abnormal clotting as well as inflammation. They believe this antibody could be a promising method for slowing or preventing cognitive decline to improve the quality of life of many MCI and Alzheimer’s disease patients in the future.
SHARE
DOWNLOAD E-BOOK
REFERENCE
https://doi.org/10.33548/SCIENTIA819
MEET THE RESEARCHER
Dr. Erin H. Norris
Patricia and John Rosenwald Laboratory of Neurobiology and Genetics
The Rockefeller University
New York, New York
USA

Dr. Norris and Dr. Sidney Strickland co-run the Laboratory of Neurobiology & Genetics at The Rockefeller University
Dr. Erin Norris completed her BA in Biology with a Minor in Chemistry at Franklin & Marshall College in Pennsylvania. She then went on to earn a PhD in Pharmacological Sciences at the University of Pennsylvania and completed her postdoctoral training at The Rockefeller University. She has undertaken numerous lecturing and research roles, as well as scientific journal editing positions. Currently, Dr. Norris is a Research Associate Professor in the Laboratory of Neurobiology & Genetics at The Rockefeller University in New York. She carries out research investigating the role of vascular dysfunction in Alzheimer’s disease pathophysiology and how it can be used to develop novel biomarkers and therapeutics. Supported by significant and prestigious funding, Dr. Norris has published over 50 peer-reviewed articles to date and is a popular invited speaker at international scientific meetings and conferences.
CONTACT
E: erin.norris@mail.rockefeller.edu
W: https://www.rockefeller.edu/our-scientists/research-affiliates/10058-erin-norris/
Twitter: https://twitter.com/ErinNor22331025
FUNDING (Past and Present)
National Institutes of Health (NIA, NINDS and NCATS)
Robertson Therapeutic Development Fund
Alzheimer’s Drug Discovery Foundation
Cure Alzheimer’s Fund
American Heart Association
Sackler Center for Biomedicine and Nutrition Medicine/Sackler Foundation
FURTHER READING
ZL Chen, PK Singh, K Horn, et al., Anti-HK antibody reveals critical roles of a 20-residue HK region for Aβ-induced plasma contact system activation, Blood Advances, 2022, 6(10), 3090–3101. DOI: https://doi.org/10.1182/bloodadvances.2021006612
PK Singh, A Badimon, Z-L Chen, et al., The contact activation system and vascular factors as alternative targets for Alzheimer’s disease therapy, Research and Practice in Thrombosis and Haemostasis, 2021, 5(4), 12504. DOI: https://doi.org/10.1002/rth2.12504
PK Singh, Z-L Chen, D Ghosh, et al., Increased plasma bradykinin level is associated with cognitive impairment in Alzheimer’s patients, Neurobiology of Disease, 2020, 139, 104833. DOI: https://doi.org/10.1016/j.nbd.2020.104833
PK Singh, Z-L Chen, S Strickland, EH Norris, Increased Contact System Activation in Mild Cognitive Impairment Patients with Impaired Short-Term Memory, Journal of Alzheimer’s Disease, 2020, 1–7. DOI: https://doi.org/10.3233/JAD-200343
Z-L Chen, P Singh, J Wong, et al., An antibody against HK blocks Alzheimer’s disease peptide β-amyloid−induced bradykinin release in human plasma, Proceedings of the National Academy of Sciences, 2019, 116(46), 22921–22923. DOI: https://doi.org/10.1073/pnas.1914831116
H Yamamoto-Imoto, D Zamolodchikov, Z-L Chen, et al., A novel detection method of cleaved plasma high-molecular-weight kininogen reveals its correlation with Alzheimer’s pathology and cognitive impairment, Alzheimer’s & Dementia: Diagnosis, Assessment & Disease Monitoring, 2018, 10, 480–489. DOI: https://doi.org/10.1016/j.dadm.2018.06.008
Z-L Chen, AS Revenko, P Singh, et al., Depletion of coagulation factor XII ameliorates brain pathology and cognitive impairment in Alzheimer disease mice, Blood, 2017, 129(18), 2547–2556. DOI: https://doi.org/10.1182/blood-2016-11-753202

REPUBLISH OUR ARTICLES
We encourage all formats of sharing and republishing of our articles. Whether you want to host on your website, publication or blog, we welcome this. Find out more
Creative Commons Licence (CC BY 4.0)
This work is licensed under a Creative Commons Attribution 4.0 International License. 
What does this mean?
Share: You can copy and redistribute the material in any medium or format
Adapt: You can change, and build upon the material for any purpose, even commercially.
Credit: You must give appropriate credit, provide a link to the license, and indicate if changes were made.
SUBSCRIBE NOW
Follow Us
MORE ARTICLES YOU MAY LIKE
Professor Abraham P. Lee | Delivering Cancer Immunotherapy with Acoustic-Electric Precision, AESOP’s Fact not Fable
Chimeric Antigen Receptor (CAR) T-cell therapy offers life-saving potential, particularly against blood cancers, but severe side effects such as cytokine release syndrome (CRS) limit its safety. These toxicities are linked to uncontrolled CAR expression levels on the T-cell surface. Led by Professor Abraham P. Lee, researchers at the University of California, Irvine, have developed an advanced microfluidic system, called the Acoustic-Electric Shear Orbiting Poration (AESOP) platform, to precisely control the dose of genetic material delivered into primary T cells. This innovation promises safer, more homogeneous, and highly effective cellular immunotherapies.
Dr Suzanne Coyle | Weaving Spirituality into Psychotherapy: How Stories Help Healing
As the practice of psychotherapy increasingly embraces the spiritual dimensions of the human experience, therapists are investigating new ways to weave faith and meaning into healing. Dr Suzanne Coyle, a licensed pastoral counsellor and family therapist, explores the role of spirituality in psychotherapy and how this intersection can support the journey of healing. Her work provides practitioners with the tools and knowledge to integrate spirituality meaningfully into clinical practice.
Dr Bo Song | Light, Energy, and the Living Nerve
At University of Shanghai for Science and Technology, recent work by Professor Bo Song and colleagues suggests that light may play an unexpected role in the way our nerves use and transmit energy. Their research explores how mid-infrared photons, tiny packets of light released by chemical reactions inside nerve cells, might interact with the fatty myelin sheath tasked to insulate axons. Together, the studies propose a new view of biological communication —one that combines chemistry, physics, and quantum mechanics— to explain how the nervous system could use light to enhance energy efficiency and information transfer.
Dr Ray Stewart | Barriers to Dental Care for People with Special Needs: A Crisis of Neglect and Inaction
For people with special healthcare needs, something as basic as visiting a dentist can be nearly impossible. A ground-breaking paper by researchers at the University of California, San Francisco (UCSF) exposes the scale of this crisis. By outlining potential paths forward, Dr Ray Stewart and Dr Ben Meisel offer hope for significant improvements in access to essential dental care.