Simphotek: Shedding Light on New Cancer Treatments
The use of radiation therapy to treat cancer has improved the long-term outcome of thousands of patients but is associated with serious side effects. Photodynamic therapy (PDT), a targeted light-based technique, has been approved as an effective treatment for some forms of cancer with fewer side effects than radiotherapy. However, the effectiveness of this technique depends on fine-tuning its application to the patient. Simphotek, a US-based company founded by world leaders in biophysics and computer modelling, together with its National Institutes of Health joint grant collaborative partners at Roswell Park Comprehensive Cancer Center and the Perlman School of Medicine, University of Pennsylvania, is focused on expanding novel technologies of PDT as a cancer treatment for solid tumours.
Novel Cancer Treatments
Cancer is one of the leading causes of death worldwide. In the UK alone, around 164,000 people die from cancer each year, accounting for more than a quarter of deaths nationwide. Traditional treatments, such as surgery, radiotherapy and chemotherapy have demonstrated success in reducing cancer mortality but are associated with major side effects as well as the recurrence of cancer.
In order to circumvent these difficulties, novel cancer therapies are being investigated that might be able to target tumours directly without causing serious side effects or damage to the surrounding tissue. A promising recent development for solid tumours is the use of photodynamic therapy, or PDT. PDT uses a drug called a photosensitiser and light to kill tumour cells.
During the procedure, the photosensitiser is injected into the bloodstream and absorbed by cancer cells in the body. The photosensitiser is completely non-toxic until exposed to certain frequencies of light, at which point it generates toxic reactive oxygen species that can kill cells. To allow time for the photosensitiser to reach the tumour, the treatment is started a few hours after injection. Exposing the tumour to light causes the photosensitiser to produce toxic reactive oxygen species that kill the tumour cells, while the healthy cells that are not exposed to light are not affected. Unlike x-ray radiation, the therapy can be repeated as many times as needed to treat the tumour.
Although PDT has been shown as an effective and targeted therapy for some superficial cancers and has been approved by the FDA for the treatment of some forms of oesophageal and bronchial cancer, it is not approved for solid cancers such as those of the brain, pancreas, head and neck, lung, and prostate. Moreover, the effectiveness of PDT depends on several factors including light power, photosensitiser concentration, and the duration of the treatment. The magnitudes of these factors are all interdependent and cannot be determined solely by clinical trials. In fact, advanced mathematical calculations and novel computing devices are required.

Dosie™ for the application of photodynamic therapy. Credit Simphotek, Inc.
Perfecting PDT
Simphotek is an organisation focused on developing novel products to aid researchers and clinicians in the study and practice of light-based therapies including cancer. Led by Dr Mary Potasek, Dr Gene Parilov, and Dr Karl Beeson, they have developed innovative medical computational dosimetry and treatment planning tools for light-based cancer treatments with the aim of improving patient outcomes following PDT by applying accurate, real-time modelling and monitoring techniques. Together with their world-leading medical collaborators, funded by joint National Institutes of Health grants, who focus on light delivery systems, their combined innovations allow clinicians to better plan, deliver, and monitor PDT. The team is also working on optimising the PDT process using computer software that can process information from the procedure and use it to fine-tune the operation in real-time.
High Definition Dosimetry
One of the major advances in the application of PDT made by Simphotek is a device called Dosie™, which is composed of Trade-Secret protected software, tuned to specific high-performance computational hardware. Dosie uses simulations of light distribution and photosensitiser concentration to inform oncologists in their planning of PDT. Dosie’s dosimetry software allows the calculation of the effective treatment dose. A similar technique is used during radiotherapy, where dose monitoring is used to limit the patient’s exposure to harmful ionising radiation while ensuring the tumour is adequately irradiated.
The current approach to determining the treatment dose for PDT is through monitoring only the total dose of light given to the patient. However, this does not necessarily correlate with the efficacy of the treatment. The outcome of PDT also depends on the concentration of the photosensitiser in the tumour, which may not be uniformly distributed within the patient and can vary from patient to patient and even between different types of tumour, and the local concentration of reactive oxygen species in the tumour produced during therapy.
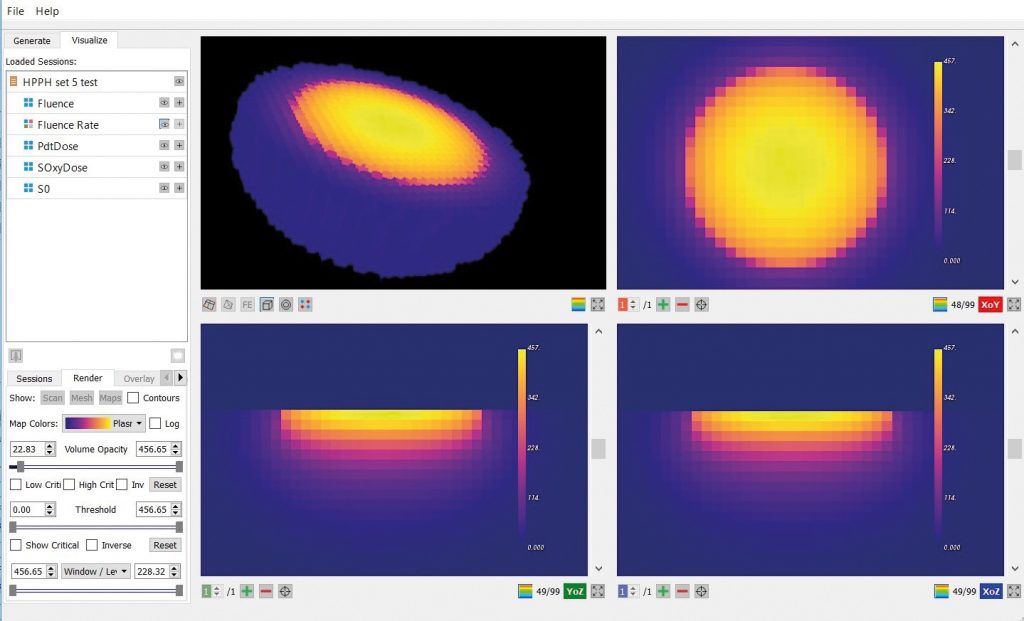
Dosie™ output. Credit Simphotek, Inc.
To more accurately determine the effectiveness of the planned therapy, Dosie takes into account the tumour shape with its optical properties and photosensitiser concentration and predicts the required amounts of the light power and treatment time. Using existing data on how well the photosensitiser can produce reactive oxygen species from the local oxygen concentration, Dosie can predict the final dose of toxic reactive oxygen species produced within the tumour to give a much better idea of how effective the treatment will be. These measures are better than simply using the dose of light administered to the tumour because they account for the availability and unevenness of the photosensitiser and oxygen across the tumour.
The data input to Dosie includes parameters specific to the patient, including the shape of the tumour, data about how well light can travel through it, local oxygen concentrations, and the concentration of photosensitiser across the tumour and surrounding tissue. Therefore, it effectively allows the treatment to be personalised to the patient. Currently, the same treatment is given to all patients with a certain indication resulting in less than optimal treatment.
As well as aiding planning, these simulations can be run in near real-time and aid the surgeon in the operating room while actually performing the treatment. Using three-dimensional dose maps defined by Dosie of the tumour, the surgeon can spot areas that are receiving an insufficient or excessive dose and adjust the light intensity or treatment time accordingly. This can reduce damage to surrounding tissue while ensuring that the tumour receives an adequate dose for effective treatment. Dosie uses multi-core CPU architecture and massive parallel GPU architecture to enable simulation and modification to be carried out in the clinic as the patient is undergoing treatment. This rapid analysis is unique to Dosie.
Drs Beeson, Parilov, and Potasek published a proof-of-concept study in the Journal of Biomedical Optics showing that Dosie predictions of reactive oxygen species correlated closely with measurements and PDT outcomes. They showed that these measurements were more reliable in predicting the outcome of PDT than existing commonly used techniques that use the dose of light administered to the tumour.
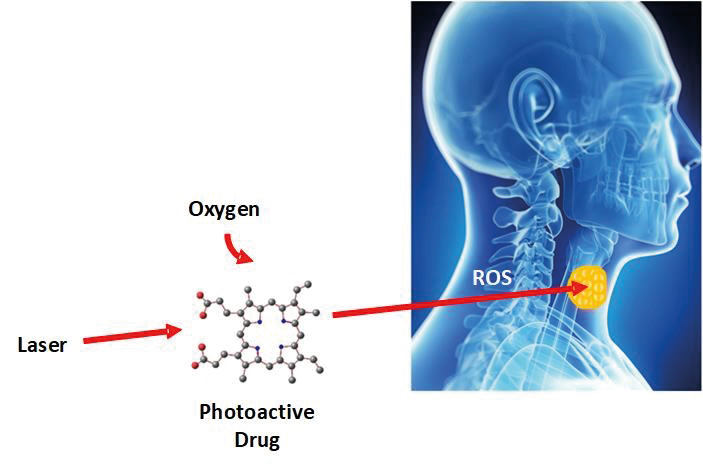
In photodynamic therapy, light interacts with a photo-active drug and oxygen to generate highly reactive oxygen species (ROS) that locally kill cancer cells in solid tumours. Credit Simphotek, Inc.
In-depth, Real-time
For tumours on the skin, an external laser can illuminate the tumour. For internal, hard to reach cancers, one or more optical fibres may be needed to deliver light to the tumour through a process known as interstitial PDT, or I-PDT, a light delivery method used at, for example, Roswell Park Comprehensive Cancer Center. Although the FDA has approved PDT for the treatment of some superficial cancers, I-PDT has not yet been approved for use in internal solid tumours, although clinical trials have shown it is effective at treating some types of cancer.
In order to advance the journey of PDT into the clinic, Simphotek is investigating patent-pending technology from its collaborators, as well as its own, to develop a clinical and operating room cancer treatment system known as INTELLI. The idea behind INTELLI is that it will be able to automatically calculate where laser fibres should be placed in order to deliver adequate treatment throughout the tumour. Additionally, Simphotek is creating new software to monitor treatment during the cancer operation and automatically control the laser light, again using real-time PDT dose calculations in Dosie.
Simphotek hopes that this complete automated bench-top system will be able to assist clinical trials into PDT for deep-seated tumours of more than 10mm thickness. A major advancement of Dosie software is that light simulations can be completed and repeated many times during the treatment, as opposed to the current simulation time of many minutes or longer.
Successful Systems
Through joint National Institutes of Health grants with the Perlman School of Medicine, University of Pennsylvania, Simphotek is also focused on delivering a complete dosimetry solution for PDT of tumours located in the body cavities, a technique known as intracavitary PDT. By combining patent-pending cutting-edge optical hardware from the Perlman School of Medicine, University of Pennsylvania, with real-time Dosie software, the Perlman School of Medicine and Simphotek are proposing a novel technology named PEDSy – the PDT Explicit Dosimetry System.
The major innovation of PEDSy is that it will be able to monitor both light dose and photosensitiser concentration in real-time from eight places in the tumour, combining these measures to interpret the ‘PDT dose’ across the tumour. The proposed PEDSy system will use eight light detectors and eight spectrometers attached to the tumour that can measure the light dose and the dose of the photosensitiser across the tumour, respectively. The latter monitors photosensitiser concentration and photobleaching, based on the measurements of the fluorescent light.
Early clinical work with a prototype of the system is focused on monitoring treatment in patients undergoing PDT for mesothelioma, a lung cancer that is difficult to treat using other methods. Currently, mesothelioma has a very poor survival rate, with most patients only surviving for 12–18 months. However, recent studies by the Perlman School of Medicine, University of Pennsylvania, have shown that even an early prototype of PEDSy can increase the median survival by nearly three years. Animal studies have shown that the efficacy of PDT can be improved by a factor of 2–4 when using ‘PDT dose’ to monitor the treatment. This could translate to an even better prognosis for mesothelioma patients treated with PDT when the PEDSy system is fully developed and used as a guiding medical system and during PDT treatment sessions.

PDT in the Operating Room. Reprinted from Evaluation of Light Fluence Distribution Using an IR Navigation System for HPPH-mediated Pleural Photodynamic Therapy (pPDT) by TC Zhu et al, 2020, Photochemistry and Photobiology, 96(2), 310–319. Copyright 2019 by John Wiley and Sons.
Photodynamic Futures
In addition to assisting with existing clinical applications of PDT, the groups are also hoping to explore novel combination treatments using PDT technology. PDT leads to necrosis and apoptosis resulting in cell death. The necrotic cells swell and disrupt the plasma membrane resulting in the release of intracellular molecules. The tumour cell develops acute local inflammation that leads to the influx of neutrophils and dendritic cells, and activates the adaptive immune response as well. As a result, PDT engages both innate and adaptive immune responses.
Major advances in immuno-oncology have seen the use of therapeutic monoclonal antibodies such as checkpoint inhibitors that can specifically target cancer cells and label them for killing by the body’s immune system. Bioconjugates of photosensitisers with antibodies such as anti-cetuximab have been used with PDT. Recent studies have shown that this combination can be even more effective in clearing cancer cells than either technique alone. In addition, nanoparticle-based PDT has been used with checkpoint blockade immunotherapy and has shown positive results.
Through creating novel dosimetry and treatment monitoring software for PDT, Simphotek is working to make PDT as commonplace as x-ray radiation therapy is today. Together with their academic partners, they are aiming to develop more accurate dosimetry hardware and software capable of making PDT a routine procedure, avoiding the complications of chemotherapy, radiotherapy, and surgery.
Reference
https://doi.org/10.33548/SCIENTIA434
Meet the researchers
Simphotek Medical Devices, Inc
Newark, NJ
USA

Dr Mary Potasek, PhD
Co-founder and Chief Scientific Officer
Dr Mary Potasek received her PhD in physics from the University of Illinois before going on to fellowships at Princeton University and the Max Planck Institute. She has held research professorships at both Columbia University and New York University, with work focusing on molecular models, nanotechnology, biophotonics, and photomedicine. In addition to her renowned research work, she has extensive experience in finance and entrepreneurship, and in 2016 was selected as one of NJBiz’s Best Fifty Women in Business.
CONTACT
E: mpotasek@simphotek.com
W: https://www.linkedin.com/in/mpotasek/
Twitter: http://twitter.com/simphotek
Dr Gene Parilov, PhD
Co-founder and Chief Technology Officer
Dr Gene (Evgueni) Parilov received his PhD in computer science from Courant Institute, New York University and has over 20 years of experience in mathematical modelling and optimisation, advanced real-time computer graphics, computational dosimetry and developing academic and industrial simulation software. In addition to his academic success, his career has included the role of marketing and sales manager for L’Oreal (Paris). He has over 25 technical publications in photonics and image processing, and has two issued patents. Dr Pariov also holds a black belt in Taekwondo.
CONTACT
E: gene@simphotek.com
W: https://www.linkedin.com/in/gparilov/
Twitter: http://twitter.com/simphotek
Dr Karl Beeson, PhD
Co-founder and Vice President
Dr Karl Beeson received his PhD in physics and has over 20 years of product development experience, with stints in industry at Allied/Honeywell and Corning, leading product design and device development. Dr Beeson has prior experience in entrepreneurship, co-founding Goldeneye Inc, a company specialising in LED sources. He is listed on 67 US patents and has published over 40 technical papers.
CONTACT
E: beesonk@simphotek.com
Twitter: http://twitter.com/simphotek
W: https://www.linkedin.com/in/karl-beeson-133b7850/
CONSULTANTS/BUSINESS ADVISORY BOARD
Dr Christopher Schaber, PhD
Dr Salvatore DeSena, MD, MBA
Dr Susan Alpert, MD, PhD
KEY COLLABORATORS
Dr Tim Zhu, Dr Keith Cengel and Dr Theresa Busch, University of Pennsylvania, Philadelphia, PA
Dr Gal Shafirstein, Roswell Park Comprehensive Cancer Center, Buffalo, NY

Creative Commons Licence
(CC BY 4.0)
This work is licensed under a Creative Commons Attribution 4.0 International License. 
What does this mean?
Share: You can copy and redistribute the material in any medium or format
Adapt: You can change, and build upon the material for any purpose, even commercially.
Credit: You must give appropriate credit, provide a link to the license, and indicate if changes were made.
More articles you may like
Dr Yurii V. Geletii – Professor Craig L. Hill | Redox Buffers: Self-Regulating Catalysts for Chemical Oxidation
Chemical reactions often demand precise control over their operating conditions to proceed efficiently. While chemists routinely use pH buffers to stabilise acidity levels, far less attention has been directed towards stabilising the electrochemical potential of solutions during oxidation–reduction reactions.
At Emory University, Dr Xinlin Lu, Dr Yurii Geletii, and Prof Craig Hill have pioneered a catalytic system that not only drives chemical reactions, but also acts as its own redox buffer. By automatically maintaining conditions optimal for electron transfers while converting malodorous thiols into odourless compounds, this innovation points to a new generation of catalysts that adjust themselves, delivering both efficiency and environmental benefits.
Dr Marie-Lou Gaucher | Unravelling Necrotic Enteritis in Poultry: The Quest for an Effective Vaccine
Avian necrotic enteritis (NE) is one of the most significant intestinal diseases affecting poultry worldwide, particularly broiler chickens. It causes major economic losses due to reduced growth rates, poor feed efficiency, and high mortality. The disease is caused by the bacterium Clostridium perfringens, specifically pathogenic type G strains. Dr Marie-Lou Gaucher from the Université de Montréal and her collaborators have been relentlessly studying ways to develop an effective vaccine against C. perfringens. Their promising findings may lead to innovative vaccination strategies and new methods to manage NE in poultry flocks.
Nick Martin | Data Assimilation: Overcoming AI’s Data Uncertainty Limitations for Water Resources
Water resources are essential for human life. Knowing how to manage water, both now and in the future, is necessary to continue using it as well as possible. Nick Martin and Jeremy White are examining limitations to artificial intelligence applications in water resources generated from noisy and estimated data sets. For poor quality data sets, they found that machine learning models will perform poorly relative to tools that explicitly include physics-based descriptions of physical processes; this is because physics-based calculations can use both data and physics knowledge through data assimilation techniques.
Professor Abraham P. Lee | Delivering Cancer Immunotherapy with Acoustic-Electric Precision, AESOP’s Fact not Fable
Chimeric Antigen Receptor (CAR) T-cell therapy offers life-saving potential, particularly against blood cancers, but severe side effects such as cytokine release syndrome (CRS) limit its safety. These toxicities are linked to uncontrolled CAR expression levels on the T-cell surface. Led by Professor Abraham P. Lee, researchers at the University of California, Irvine, have developed an advanced microfluidic system, called the Acoustic-Electric Shear Orbiting Poration (AESOP) platform, to precisely control the dose of genetic material delivered into primary T cells. This innovation promises safer, more homogeneous, and highly effective cellular immunotherapies.