Dr Sandra Grumelli | The Importance of the Choline in Chronic Lung Infections
Article written by Helen Rickard, PhD
People with chronic lung conditions like COPD and cystic fibrosis are vulnerable to lung infections caused by the bacterium Pseudomonas aeruginosa. These infections are often difficult to treat and can cause sudden worsening of symptoms, known as flare-ups or acute exacerbations. While we know P. aeruginosa triggers inflammation and damage in the lungs, much less is understood about how exactly it causes these flare-ups, or how it survives in such a harsh environment. Dr Sandra Grumelli from the Center of Investigations of Respiratory Diseases in Argentina, has explored the role of a common molecule called choline which is released during infection. Using a combination of mouse models and laboratory experiments, she has discovered that choline not only makes breathing harder, it also helps P. aeruginosa adapt to and persist in the lungs. Her research opens up new possibilities for tackling chronic infections by targeting the bacteria’s energy use and the way it responds to its environment.
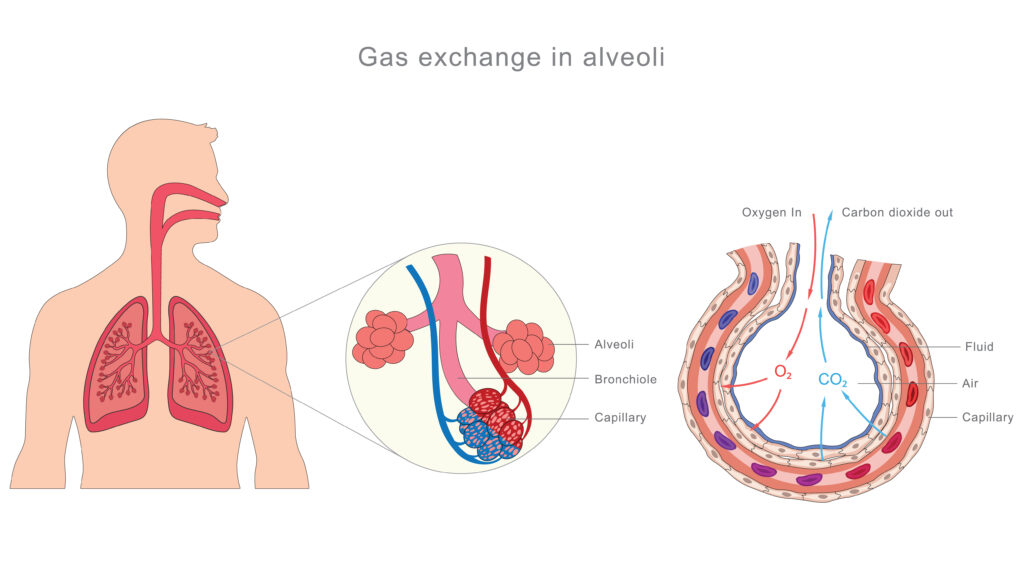
Chronic Obstructive Pulmonary Disease
Chronic obstructive pulmonary disease (commonly known as COPD) is the name for a group of lung conditions that cause breathing difficulties. These conditions include emphysema, where the air sacs in the lungs called alveoli disappear. The walls in these sacs are usually stretchy, allowing them to fill with air. In people with COPD, it is harder for these sacs to inflate and deflate, causing difficulties with breathing. Another aspect of COPD is chronic bronchitis, when the lining of the airway becomes irritated and inflamed, leading to cough and overproduction of mucus.
In the United States COPD affects more than 14 million people and is the sixth leading cause of death, according to the Centers for Disease Control and Prevention. The most common COPD symptoms are shortness of breath, a persistent cough, and feeling very tired. COPD symptoms can suddenly get worse for a few days, known as flare ups or acute exacerbation which often need additional treatment. COPD happens when the lungs become damaged and inflamed often due to smoking, air pollution, or a genetic mutation. There is currently no cure or way to reverse COPD damage to the lungs because the air sacs disappear, but steroids and oxygen can help people through flare-ups.
During flare ups people may cough more, produce more mucus, struggle to breathe, and have to breathe faster to get enough oxygen. Normally the physical process of breathing uses only a little bit of the body’s oxygen (about 5%), but during a flare up it can take a lot more effort (up to 250%) and oxygen just to keep breathing. This is partly because during a flare up there is more tissue resistance and the lungs can’t breathe out carbon dioxide properly, causing it to build up the blood in a process called hypercapnia which makes the blood more acidic.
Cystic Fibrosis
Another condition which can lead to breathing difficulties, persistent coughs, and frequent lung infections is cystic fibrosis. This is a genetic condition, where a faulty gene is passed down by both parents, resulting in the production of thick mucus which affects the lungs and other body systems. Cystic fibrosis also currently has no cure, but similarly to COPD, treatments including steroids and inhaled medicines which widen the airways can improve respiratory symptoms.
Pseudomonas aeruginosa and Lung Diseases
Both COPD and cystic fibrosis make people more vulnerable to bacterial infections of the lungs and respiratory tract. A key bacterial species which can cause these infections is Pseudomonas aeruginosa (P. aeruginosa), this bacterium can cause infections in all parts of the body including the skin and gut but is notorious for causing hard to treat infections in people with underlying respiratory conditions.
Up to 20% of people diagnosed with COPD are infected with P. aeruginosa, and P. aeruginosa is the leading cause of lung infections in people with cystic fibrosis. Infection by P. aeruginosa in people with lung conditions can lead to a decline in lung function, increased symptom flare ups, and is associated with worse clinical outcomes and reduced lifespan. P. aeruginosa is able to release harmful substance within the lungs and respiratory tract during infections. The outer surface of the P. aeruginosa bacteria includes molecules called lipopolysaccharide or LPS, these trigger our immune system leading our body to release inflammatory molecules and enzymes which can further damage lung tissues and contribute to worsening of respiratory symptoms.
Despite being so hard to treat and a major caused of illness, little is known about how P. aeruginosa causes severe lung disease acute exacerbation. Dr Sandra Grumelli has led a team of expert researchers at the CIMeR in Argentina alongside scientists at Harvard Medical School to understand the molecular mechanisms between P. aeruginosa and lung disease symptoms.
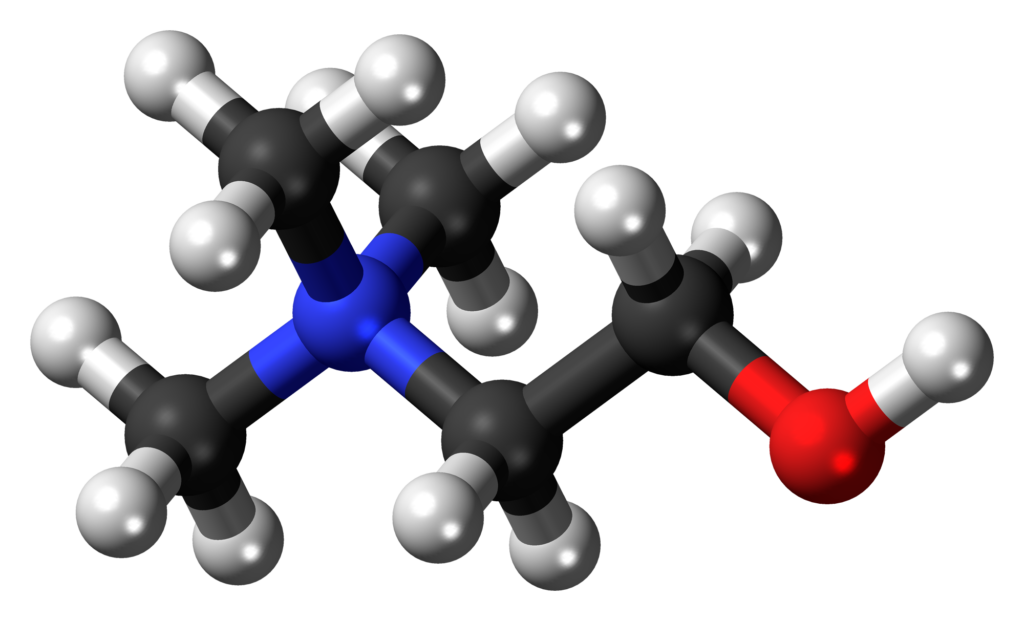
Choline
The Importance of Choline
Choline is a naturally occurring molecule found in the membranes around cells and in surfactant, the slippery substance which helps keep our lungs open. As well as its LPS triggering the immune system, P. aeruginosa can also produce enzymes which break down the lung surfactant, as this breaks down it releases a molecule called choline. Choline can trigger the airways to narrow and change how blood vessels within the lungs behave, making breathing even harder.
Dr Grumelli and her team at Harvard Medical School conducted a series of experiments to find out if the production of choline by P. aeruginosa may actually be triggering the flare ups. The team used a mouse model to understand the role of P. aeruginosa in the development of respiratory flare up symptoms. First, they exposed some of the mice to cigarette smoke over time to create emphysema-like lung damage, they then added LPS from P. aeruginosa to mimic the lung inflammation that would be seen during infection to some of the mice. Choline was then given and the team conducted experiments to see how these factors affected the mouse lungs. They used a specialised machine to measure how hard the lungs had to work to breathe, including checking lung stiffness, resistance in the airways, and how much oxygen and carbon dioxide the mice were breathing in and out. They also collected lung fluid samples to count the immune cells, and looked at lung tissue under a microscope to check for damage. They measured how much energy the mice were using and how the levels of carbon dioxide and acidity in their blood changed.
The team also wanted to understand how choline impacts P. aeruginosa, so in laboratory experiments they grew the bacteria using choline and a different molecule called succinate as its food source. They then assessed the levels of key molecules within the bacterial cells and speculated how this might impact the bacteria’s behaviour within the human lung.
Dr Grumelli found that the LPS caused a strong immune reaction in the lungs, with high numbers of inflammatory cells that released enzymes and damaged tissues, this led to the breakdown of the alveoli and made the lungs less elastic. They also discovered that choline made breathing much harder, the lungs had to use more energy and oxygen to function causing carbon dioxide to build up and acidify the blood. Interestingly, the team also found that choline doesn’t just affect the lungs it also changes the bacteria, exposure to choline caused P. aeruginosa in the lab test to produce more LPS which would allow it to stick to and damage lung tissues. It also caused the bacteria to reduce its energy needs giving it a survival advantage in the lung.
Polyphosphate Production
These findings suggested that treating people with P. aeruginosa lung infections with succinate, may reduce the symptoms associate with choline and make the infections easier to treat. To understand more about how choline impacts P. aeruginosa in lung infections the team in Argentina expanded on their previous experiments and grew the bacteria in the lab using choline as its main energy source and compared it to bacteria grown with succinate.
Dr Grumelli discovered that choline caused the bacteria to switch into a survival mode, building up large amounts of a compound called polyphosphate which helps bacteria handle stress, resist attack by the body’s immune systems, and be able to persist in the lungs for longer periods of time. They also found that an enzyme called polyphosphate kinase was much more active in the choline fed bacteria, while the enzyme polyphosphate phosphatase, which breaks down the polyphosphate, became less active. This resulting in the bacteria being able to build up large stores of polyphosphates and produce more LPS.
The laboratory tests showed that the bacteria grown with choline made less energy, but this allowed them to become more efficient. As they used less oxygen, they were also more able to survive in the low oxygen environment found within damaged lungs.
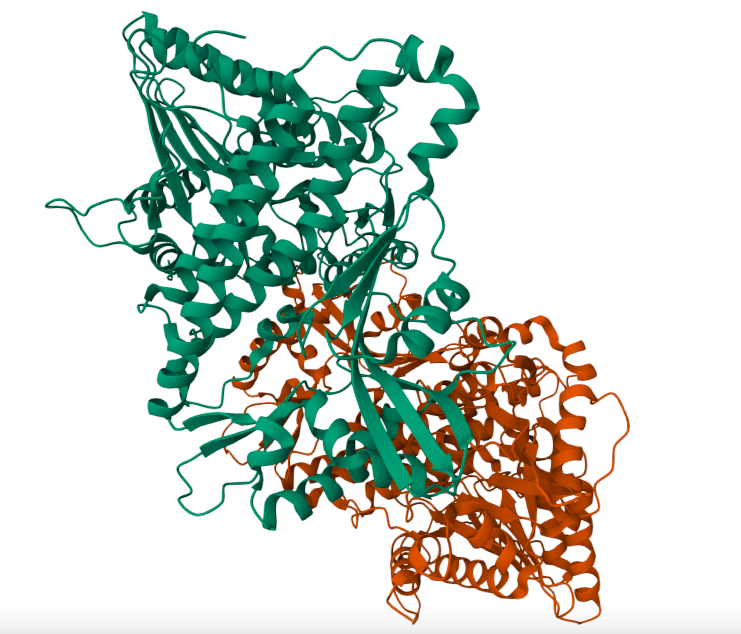
Polyphosphate kinase
What This Research Could Mean for Patients
Dr Grumelli’s work provides exciting insights into why P. aeruginosa infections are so difficult to manage in people with chronic lung conditions such as COPD and cystic fibrosis. Their work reveals that choline, a molecule naturally found in our lungs, plays a surprising double role as it not only makes breathing harder for patients during flare ups, but it also helps the bacteria survive and cause more damage.
This research highlights the potential for possible new treatment strategies. For example, targeting the bacterial enzymes that respond to choline, or changing the nutrients available in the lungs could reduce the severity of infections and improve patient outcomes. Dr Grumelli’s findings may lead to therapies that go beyond antibiotics and support people living with chronic hard to treat lung infections.
SHARE
DOWNLOAD E-BOOK
REFERENCE
https://doi.org/10.33548/SCIENTIA1284
MEET THE RESEARCHER

Dr Sandra Grumelli
Centro de Investigación en Medicina (CIMeR), Universidad Católica de Córdoba, Argentina
Dr Sandra Grumelli is a biomedical scientist with over two decades of experience in respiratory research, translational science, and immunology. She obtained her PhD in Biology from the National University of Río Cuarto in Argentina, followed by extensive postdoctoral training at leading institutions including Baylor College of Medicine and Harvard Medical School. Her research has focused on chronic lung diseases, particularly the immune and metabolic interactions between Pseudomonas aeruginosa and the human host in cystic fibrosis and COPD. Dr Grumelli has held research and teaching appointments in Argentina and the USAle, led projects funded by Tufts University and the American Thoracic Society, and received multiple international fellowships and travel awards. Dr Grumelli is also a science communicator, peer reviewer for leading journals including PLOS ONE and FEMS, and currently serves as an editor for The Journal of Disease. She combines her scientific background with certified training in medical interpretation to help bridge communication in clinical and research settings.
CONTACT
E: sgrumelli@yahoo.com
KEY COLLABORATORS
Alejandro Rossi from Rizobacter
FUNDING
CONICOR 72/95, 252/96, 417/97, 1380/97
CABBIO
UNRC Res1073, Exp57803
American Thoraxic Society
National Insitute of Health
St. Elizabeth Hospital
CIMeR
FURTHER READING
S Grumelli., Choline Triggers Exacerbations of Chronic Obstructive Pulmonary Disease in Patients Infected with Pseudomonsa aeruginosa, Current Respiratory Medicine Review, 2016, 12(2) 167-174. DOI: https://doi.org/10.2174/1573398X12999160506104327
S Grumelli, A Rossi., Bioenergetics of the Polyphosphates Accumulation in Pseudomonas aeruginosa via Polyphosphate Kinase Activation by Choline in a Lung Colonization Model, Heliyon, 2023, 9(2). DOI: https://doi.org/10.1016/j.heliyon.2022.e12601


REPUBLISH OUR ARTICLES
We encourage all formats of sharing and republishing of our articles. Whether you want to host on your website, publication or blog, we welcome this. Find out more
Creative Commons Licence (CC BY 4.0)
This work is licensed under a Creative Commons Attribution 4.0 International License. 
What does this mean?
Share: You can copy and redistribute the material in any medium or format
Adapt: You can change, and build upon the material for any purpose, even commercially.
Credit: You must give appropriate credit, provide a link to the license, and indicate if changes were made.
SUBSCRIBE NOW
Follow Us
MORE ARTICLES YOU MAY LIKE
Professor Abraham P. Lee | Delivering Cancer Immunotherapy with Acoustic-Electric Precision, AESOP’s Fact not Fable
Chimeric Antigen Receptor (CAR) T-cell therapy offers life-saving potential, particularly against blood cancers, but severe side effects such as cytokine release syndrome (CRS) limit its safety. These toxicities are linked to uncontrolled CAR expression levels on the T-cell surface. Led by Professor Abraham P. Lee, researchers at the University of California, Irvine, have developed an advanced microfluidic system, called the Acoustic-Electric Shear Orbiting Poration (AESOP) platform, to precisely control the dose of genetic material delivered into primary T cells. This innovation promises safer, more homogeneous, and highly effective cellular immunotherapies.
Professor Loren Babcock | The Race to Save Fossils From the Hands of Time
Ohio Wesleyan University’s geological collection, which was amassed in Delaware, Ohio, USA, is among the oldest in America, but decades after those who assembled the collection retired and passed on, the collection fell into obscurity and its storage area was repurposed. Prof Loren Babcock, Director of the Orton Geological Museum at The Ohio State University, is leading a 3-year rescue project to stabilise, catalogue, and digitise more than 15,000 specimens. From rediscovered scientific-name-bearing type fossils to ethically sourced collections linked to abolitionist networks, the initiative promises not only to safeguard irreplaceable scientific material, but to revive a once overlooked foundation of American geology for future generations.
Professor Dilip Kumar | From the Ground Up: The Making of a Modern Mathematics Centre in Kerala
In 1977, Professor Aleyamma George, head of statistics at Kerala University, dreamed of establishing a new centre for mathematical sciences in Kerala’s coastal capital Trivandrum. Her mission was to encourage talented young mathematicians to engage in frontline research in the mathematical sciences. But, for many years, it struggled to obtain regular government funding and survived only because of the Herculean efforts and personal funds of both Prof George and its Director since 1985, Professor Arak Mathai.
Later, it supported the operations of eight different dedicated research groups producing award-winning work, and regularly hosts undergraduate-level workshops; it fulfilled the original mission of training and educating new generations of mathematicians, so that they may contribute to cutting-edge, internationally recognised research.
Dr Ray Stewart | Barriers to Dental Care for People with Special Needs: A Crisis of Neglect and Inaction
For people with special healthcare needs, something as basic as visiting a dentist can be nearly impossible. A ground-breaking paper by researchers at the University of California, San Francisco (UCSF) exposes the scale of this crisis. By outlining potential paths forward, Dr Ray Stewart and Dr Ben Meisel offer hope for significant improvements in access to essential dental care.