Professor Terry Powley – The Brain and the Gut – a Meeting of Two Minds
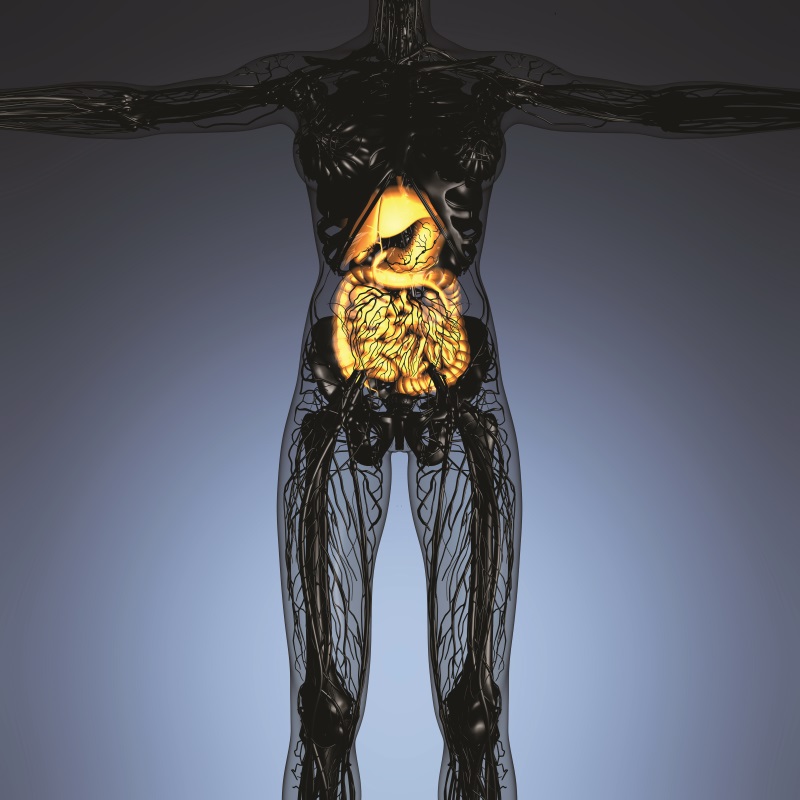
Until now, the brain and the neural network of the gastrointestinal tract have been considered largely independent organs. Recent experiments conducted by Professor Terry Powley of Purdue University and his colleagues have fundamentally challenged this belief. Their work shines much needed light on the complex neural circuitry of the stomach and intestines and will assist the development of novel and optimised therapies for problematic gastric disorders.
The Need for More Effective Gastric Treatments
In recent years, the prevalence of obesity, type II diabetes, and gastrointestinal (GI) tract disturbances, such as gastroparesis, tachygastria, and gastroesophageal reflux disease, has reached epidemic status. Although various treatments are available, these gastric disorders are either not readily addressed with surgery or they necessitate radical and irreversible surgical intervention.
The increasing burden of these disorders on people’s quality-of-life and the associated costs to the healthcare system demonstrate that there is still an urgent need for more effective treatments and therapies than those that currently exist. To date, gastric interventions have largely been developed using incomplete descriptions of the distribution of nerves (the innervation) to the GI tract. Essential information on the neural circuitry of peripheral organ-systems is critically needed if more efficacious therapies are going to be developed and optimised.
Challenging the Classical View
Classically, the brain and the enteric nervous system (the mesh-like neuronal network in the gut wall that governs the GI tract) have been considered largely independent neural organs in regards to ingestion and digestion, with the brain being responsible for the ‘what’, ‘when’, ‘where’ and ‘how’ to eat and the ‘little brain’ in the gut working to process the nutrients that arrive in the stomach. Very few individual neurons interconnect the two ‘brains’, which led researchers to assume that the two neural organs were relatively autonomous.
‘The limited numbers of axons interconnecting the big brain in the head and the little brain in the gut have nerve ending specialisations that make the connecting neurites far smarter than anticipated.’
Recently, a team of researchers led by Professor Terry Powley at Purdue University in Indiana, USA, have fundamentally challenged these assumptions. By performing neural tracer and digital reconstruction experiments, Professor Powley and his colleagues have determined that although few neurons interconnect the brain and the enteric nervous system in the GI tract, those neurons prove to have extensive, complex, and highly differentiated terminal neurites – branch-like structures that are responsible for distributing information (axons) or collecting information (dendrites) over a region of the gut – which make them capable of far more coordination and communication than classically assumed.
‘The limited numbers of axons interconnecting the big brain in the head and the little brain in the gut have nerve ending specialisations that make the connecting neurites far smarter than anticipated,’ says Professor Powley.
Mapping the Stomach’s Neural Circuitry
The stomach is a key organ in the regulation and dysregulation of food intake. As the body has a basic need to be aware of ingested food, there is an intricate network of electrically excitable cells, elaborately arranged into circuits and strategically distributed throughout the gut. These circuits convert food into electrical signals coordinating motility, secretion, food intake, and even mood and other behaviours. This neural network is known as the ‘brain-gut connectome’ and is built around food sensing.
As part of the Stimulating Peripheral Activity to Relieve Conditions (SPARC) Program, Professor Powley is conducting a far-reaching experiment to trace and digitally reconstruct the ‘smart’ nerve endings of the brain-gut connectome, with the aim of addressing critical gaps in our understanding of how the connectome controls stomach function.
He has been joined in this endeavour by a team of co-investigators, comprising expert researchers from his laboratory at Purdue University in collaboration with faculty from several other Purdue laboratories, with Professor John Furness of the University of Melbourne, Australia, and Associate Professor Walter Voit from the University of Texas in Dallas, USA. Using physiological tools and stimulation techniques, this highly specialised team aim to create high-resolution maps of the stomach’s neural circuitry. These maps will hopefully be used to develop next generation neural modulation devices (implants that can stimulate nerves), which could be used as tools for developing new therapeutic strategies.
The stomach is particularly appropriate and accessible for neuromodulation (altering nerve activity by delivering electrical or pharmaceutical agents to a target area), since both regional GI nerve reflexes and the more distributed central nervous system (CNS) signals that travel between GI sites are carried in one peripheral nerve – the vagus – which possesses many branches that provide multiple candidate sites for electrode placement.
However, previous attempts to improve and monitor gastric disorders by neuromodulation have been problematic, due in part to a lack of knowledge about the vagal-stomach connectome – the neural circuit linking the vagus nerve to target organs in the GI tract.
Despite the critical roles that the stomach plays in controlling ingestion and digestion, the vagal sensory fibres that project into the gastric wall have not been thoroughly described. Although the existence of these connections has long been known and simple or generic, unmapped vagal endings have been assumed, many specific characteristics of vagal sensory and motor endings in the GI tract are still largely unknown.
The characterisation of these nerve endings has been challenging, probably because the parent fibres of the vagus nerve travel exceptionally long distances between the brain and the GI tract, passing through multiple tissues in the gut wall, and ending in copious complex arrangements (arrays). All of these details make it difficult to accurately recognise any particular nerve ending in the GI tract originating from a specified CNS source and to fully reconstruct and characterise that ending using only conventional histological techniques.
Using high definition labelling techniques, Professor Powley and his team are currently defining the unmapped elements of the vagal-stomach connectome in rats, before going on to establish a large animal pig model and, ultimately, to evaluate the circuitry in human stomachs. In the rat model, the team is defining ‘vagal intramuscular arrays’ and other specialized endings that are distributed throughout the stomach wall by a set of basic structural features. In some cases, they are modifying and adapting these ending definitions to the local tissue environments in different gastric regions.
These findings have allowed the team to more completely characterise the nerve fibres that innervate the stomach wall. It is hoped that this additional morphological information will provide greater structural detail of the gastric wall neural circuitry and, most importantly, will aid the design of future experiments that assess the physiology of the nerve fibres.
Professor Powley and his team plan to use state-of-the-art closed-loop stimulator technologies, algorithms, and electrodes to assess the reliability, validity, and stability of vagal stimulation on stomach wall and muscle activity, gastric emptying, reflux, hormone release, CNS activation, and the ingestion of meals. Their ultimate goal is to use these implantable stimulators and electrodes for human use.
Understanding the Brain-Intestine Connection
In a second experiment, funded by the National Institute of Health, Professor Powley and his team are focusing on digitising and characterising the vagal projections that allow communication between the brain and different sites along the GI tract. The vagal sensory and motor innervation of the smooth muscle tissue in the intestines is critically important for GI motility and related disorders. Also, the vagal innervation of the intestinal mucous membrane, and the layers underneath it (the submucosa), is equally important for monitoring nutrient fluxes and hormonal responses, regulating absorption, and modulating secretion.
 Furthermore, the neural activity associated with these mucosal layers is especially relevant to various eating disorders that require effective clinical interventions. However, until now, no complete three-dimensional mapping of the vagal circuitry (i.e. the endings, axons, and dendrites) in the heavily folded intestinal mucous membrane and submucosa has been accomplished.
Furthermore, the neural activity associated with these mucosal layers is especially relevant to various eating disorders that require effective clinical interventions. However, until now, no complete three-dimensional mapping of the vagal circuitry (i.e. the endings, axons, and dendrites) in the heavily folded intestinal mucous membrane and submucosa has been accomplished.
Three distinct vagal pathways – three separate higher order branches of the vagus nerve – supply the full length of the intestines. It has already been established that one (or more) nerve bundle originating from the gastric branches travels over the pylorus (the furthest part of the stomach) to reach the duodenum (the first segment of the intestines). Another bundle separates from the common hepatic branch of the vagus and joins the small intestine at the level of the duodenum, while the two ‘coeliac branches’ of the vagus take an indirect route through the connective tissue of the descending aorta, before travelling alongside neurovascular bundles to the intestines.
However, what intestinal regions and which vagal physical properties (phenotypes) are supplied by each path has never been determined. It is hoped that Professor Powley’s experiment will determine which of the three nerve branches and terminal phenotypes connect to specific regions of the intestines and will provide vital information to help design novel GI surgeries, as well as experimental gastric interventions.
In the first stage of their experiment, the team removed the entire GI tract from rats, separating the intestine from the stomach and rectum, and flushing it of all contents before dividing it into its different segments: duodenum, jejunum, ileum, cecum, and colon. Following multiple inventory screening steps, the team has been able to produce a complete sample of vagal endings and descriptively characterise those endings.
This survey of the vagal sensory innervation of the gut will allow the team to map the distribution of the nerve endings and identify any novel phenotypes and/or variants in the vicinity of the mucous membrane and submucosa. Professor Powley says, ‘we will need to identify 300–400 complete vagal endings of each type to be able to reliably recognise the distribution, regional concentrations, and specialisations of the vagal phenotypes through the GI tract.’
In the next stage of the experiment, Professor Powley and his team are performing highly selective vagotomies – removing one of the three vagal pathways to the intestines – in three different groups of rats. The brain and GI tract of each animal are then examined for characteristic patterns of loss associated with the different vagotomies. This novel procedure has permitted the accurate recording and reconstruction of vagal endings, axons, and dendrites.
Plans for the Future
There is still much that Professor Powley and his team hope to achieve, and their work in this arena is ongoing. Going forward, their research will consolidate and extend existing anatomical, molecular, and functional characterisations of the vagal-stomach connectome and locate optimal sites for disease-controlling vagal neuromodulation. Importantly, their findings will help to evaluate the best ways to manage gastric disorders, including gastroparesis, reflux disease, and eating disorders.
With regards to the vagal innervation of the intestines, questions of critical importance when designing future treatments and therapies are whether each of the three vagal pathways is responsible for the innervation of a given region of the intestine, whether there is any overlap of the distribution fields provided by the different paths, or whether each of the vagal paths represents a different phenotype.
Professor Powley and his colleagues plan to take their experiments further by determining which of the vagal branches supply which arrangements of nerve endings in the intestine smooth muscle wall. In addition, as sex differences are an important factor in vagal structure and function, the patterns and phenotypes of vagal endings in males and females will be compared.
Collectively, these ground-breaking experiments will provide much needed information on the brain-gut pathways that control how the intestines handle nutrients, illuminate the points of contact with the gastrointestinal microbiome, and greatly inform the future development of effective gastric interventions.
Meet the researcher
Professor Terry L. Powley
Department of Psychological Sciences
Purdue University
West Lafayette, IN
USA
Professor Terry Powley is a Ben J. Winer Distinguished Professor of Behavioural and Social Sciences at Purdue University in Indiana, USA. He completed his first degree at DePauw University, Indiana, before going on to complete a MS and PhD in psychology at the University of Wisconsin in 1970. He previously held the posts of Assistant Professor, and then Associate Professor of Psychology, at Yale University, USA, before retuning to Indiana to become Professor of Psychology at Purdue University in 1980. He has served on the Executive Committee of Purdue University Neuroscience Program, has been Chairman of the Program Committee of Midwestern Psychological Association and has participated as the President of the Society for the Study of Ingestive Behavior. Professor Powley has also been the recipient of numerous awards including the NIH Research Career Development Award, the NIH MERIT Award and the Master of Gastroenterology Award (life-time achievement award) from the American Gastroenterological Association. Currently, his research focuses on identifying and mapping the autonomic, endocrine, and somatic pathways involved in the control of feeding and metabolism.
CONTACT
E: powleyt@purdue.edu
T: (+1) 765 494 6269
W: https://sparc.purdue.edu/sci/terry-powley
KEY COLLABORATORS
Dr Pedro Irazoqui, Purdue University, USA
Prof John Furness, University of Melbourne, Australia
Dr Zhongming Liu, Purdue University, USA
Dr Thomas Nowak, Indiana University School of Medicine, USA
Dr Robert Philips, Purdue University, USA
Dr Bartlomiej Rajwa, Purdue University, USA
Dr Jenna Rickus, Purdue University, USA
Dr Jospeh Robinson, Purdue University, USA
Dr Walter Voit, University of Texas at Dallas, USA
Dr Matthew Ward, Purdue University, USA
FUNDING
NIH R01 grant (DK27627)
NIH SPARC grant (OT2)
REFERENCES
TL Powley, CN Hudson, JL McAdams, EA Baronowsky, RJ Philips, Vagal intramuscular arrays: the specialized mechanoreceptor arbors that innervate the smooth muscle layers of the stomach examined in the rat, Journal of Comparative Neurology, 2016, 524, 713–737.
TL Powley, RJ Phillips RJ, Musings on the wanderer: what’s new in our understanding of vagovagal reflexes? I. Morphology and topography of vagal afferents innervating the GI tract, American Journal of Physiology-Gastrointestinal and Liver Physiology, 2002, 283, G1217–G1225.