Dr Victoria Morgan – Mapping Brain Networks to Understand Epilepsy
Epilepsy is one of the most common causes of disability worldwide, but for many patients, treatment fails to be effective. Dr Victoria Morgan and her team from the Department of Radiology and Radiological Sciences at Vanderbilt University Medical Center are using functional connectivity mapping to find out why some patients respond better to treatment and what alternative ways there may be to tackle this debilitating disorder.
Epilepsy: A Global Problem
Epilepsy is a neurological disorder characterised by recurrent seizures which are the result of abnormal, synchronous firing of neurons in the brain. Under normal conditions, neurons aren’t in sync and fire when they receive signals. In epilepsy, however, changes to the threshold allowing firing can trigger mass activation of neurons and ‘bursts’ of synchronised electrical activity.
Temporal lobe epilepsy (TLE) is one of the most common forms of epilepsy. This is a type of focal epilepsy, where seizures arise from one or more discrete locations called the seizure focus. In this case, the focus is within the temporal lobe. This is in contrast to generalised epilepsy where seizures can originate from much of the brain simultaneously. The initial treatment for most patients with epilepsy is anti-epileptic drugs, which aim to dampen down the electrical hyperactivity responsible for triggering seizures. In almost 40% of patients, however, drugs fail to work or have intolerable side effects.
For focal epilepsy, the next step is to try surgery, which is often preferable to long term drug treatment anyway. When patients come into the clinic with drug-resistant focal epileptic seizures, neurologists can perform tests to attempt to identify the exact location of the seizure focus, and, in TLE, this generally tends to be the hippocampus. Surgery is then performed to remove this area. While technological advancements have continually increased our ability to accurately identify the focus, the success rate of these surgeries has not improved as we would expect. Clearly, there is something else at play.
Dr Victoria Morgan at the Vanderbilt University Institute of Imaging Science at Vanderbilt University Medical Center is using her expertise in biomedical engineering and magnetic resonance imaging (MRI) to find out why focal epilepsy is so difficult to treat. ‘Even in cases where the clinicians are most confident in the localisation of the seizure focus, the success rate is about 80%,’ explains Dr Morgan, ‘This is the mystery I am interested in solving.’
Nodes and Edges
Much effort has been put into understanding what patient variables are associated with differing surgical outcomes. In TLE affecting the hippocampus, younger age and a history of fewer tonic clonic seizures prior to surgery have been observed to correlate with success but attempts to design predictive tests have so far done little to improve results. Refining these tests would be a significant step forward for epilepsy treatment, and since brain surgery is associated with high risks it would be undesirable to perform this procedure on patients for whom it is less likely to benefit.
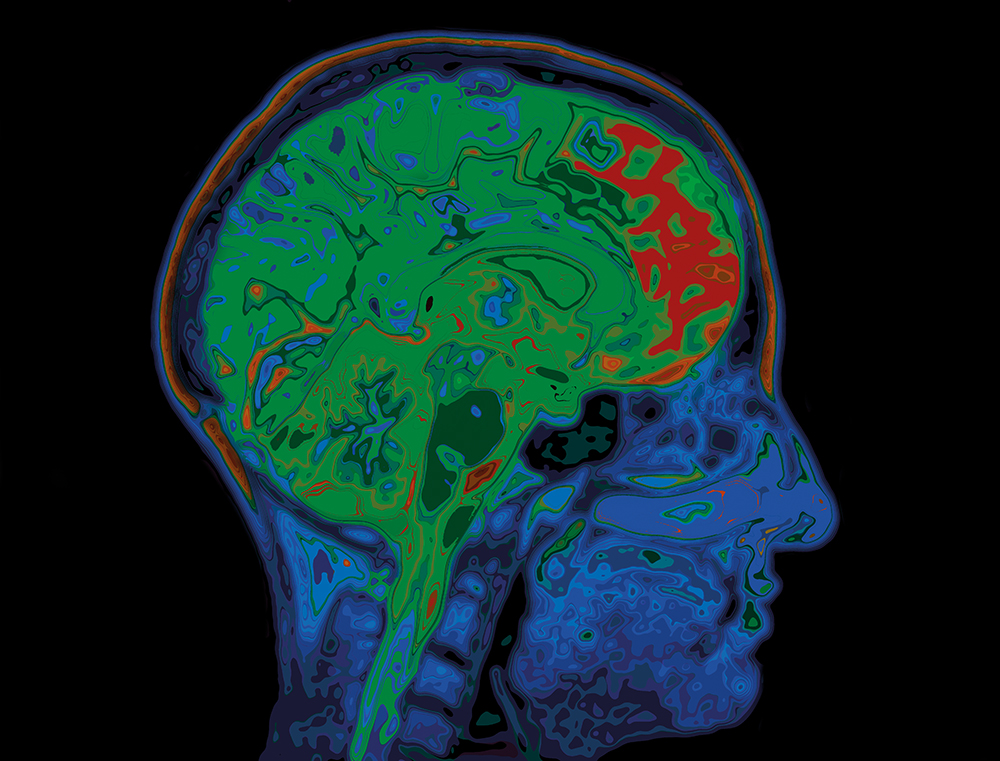
For years, scientists have been searching for the best way to visualise the brain in order to understand different disease states. With epilepsy, much of the attention has been given to the focus to try and identify how and why seizures arise. Dr Morgan, however, believes that looking at the brain as a network of interconnected points is much more useful in understanding epilepsy.
Network connectivity mapping allows the brain to be viewed as a collection of points, referred to as ‘nodes’, and the intercommunication between these nodes, called ‘edges’. By looking at the complex system formed by these nodes and edges we can learn more about how the brain acts during normal functions, such as memory retrieval or movement, and compare this to how it acts in abnormal situations, like seizures. Functional connectivity mapping relies on the use of functional MRI (fMRI), which measures changes in blood flow to different regions of the brain that correlate with changes in neuronal activity. Structural connectivity mapping uses diffusion-weighted MRI to look at how water moves along white matter tracts across the brain.
Dr Morgan’s research has suggested that while the seizure focus may be similar in groups of patients, the way that activity is propagated around this network of nodes and edges may be different. This may explain why, even when the focus is identified, surgery is ineffective.
‘Even in cases where the clinicians are most confident in the localisation of the seizure focus, the success rate is about 80%. This is the mystery I am interested in solving.’

Changing Networks
‘What makes my work unique is that I am developing a general framework around the idea that epilepsy networks evolve even before the first seizure occurs and continue to evolve over years prior to and after surgery,’ notes Dr Morgan. Using MRI, Dr Morgan and her team were able to show that epileptic patients have differences in their functional and structural connectivity networks compared to healthy controls. Identifying such a difference can allow for the development of a biomarker, a characteristic of a disease which aids in diagnosis.
Dr Morgan noted that these changes also correlated with how severe their epilepsy was and how long they had been suffering from it. This kind of analysis has been studied before and has huge potential to be used clinically to assess an individual’s disease progression. But Dr Morgan states the changes seen and the techniques used need to see improvements in sensitivity, specificity, and generalisability to be wholly useful.
Other challenges that need to be overcome are how to implement such a complex measure. Analysing networks requires replicable methods and using connectivity biomarkers is computationally intensive. In addition, results can be ambiguous or difficult for clinicians to interpret. Indeed, some studies have reported conflicting changes, with some finding increases and others finding decreases in functional connectivity between certain areas. It’s clear that connectivity mapping needs to see advancements in methods before it is used in the clinic, and Dr Morgan hopes to be the one to achieve this.

Predicting Outcomes Can Help Improve Treatment
One of Dr Morgan’s key findings is that patients whose seizures were reduced following surgery tended to share a particular network structure before they underwent the treatment. Patients with different networks were much less likely to respond in the same way and saw little or no improvement after surgery. Interestingly, in the successfully treated group, there were certain pathways in the network found to be associated with the length of time until a rare seizure occurred post-surgery. This kind of foresight provided by MRI and connectivity mapping is an invaluable tool when trying to treat such a complex neurological disease. Dr Morgan’s models were able to successfully predict which patients would be less responsive to treatment in cases where the currently used predictive models would not.
While the most desired outcome of epilepsy treatment is total remission of seizures, Dr Morgan’s model allows for a spectrum of success. Importantly, the length of time which passes before seizure recurrence may be associated with different networks and mechanisms. Earlier, severe recurrence may suggest a larger difference between their network and the success-predictive network, while later, milder recurrence may be more similar. These slight variances in networks can mean the difference between surgery which accurately targeted the epileptogenic system and focus, and that which did not.
‘Long-term outcomes years after surgery are at least partially dependent on how networks evolve after surgery,’ adds Dr Morgan. The main premise of her work is that the integrity of the seizure-associated network both before and after surgery is significant in predicting recurrence of epilepsy symptoms.
The network structure itself is unique to each patient, being affected by age, genetics, medication, and type of seizure, but general patterns can be found, nonetheless. Dr Morgan hopes to quantify this connectivity network in pre- and post-surgical patients to properly elucidate the relationship to seizures and their recurrence. ‘My hypothesis is that conventional clinical methods will be successful in patients with a specific focus and network combination,’ she elaborates. Ultimately, by identifying which networks respond to which treatments we can improve success rates and better help patients.
The Future of Epilepsy Biomarkers
Dr Morgan’s work presents an innovative new landscape for epilepsy research. Developing new biomarkers is an essential step forward in improving the way we treat epilepsy, especially biomarkers that can distinguish between different treatment outcomes. Dr Morgan also hopes to study the long-term development of seizures in humans, something which has not been studied in this way before. The characterisation of post-surgery recurrence networks is an incredibly significant finding in epilepsy research and paves the way for a new era of understanding neurological disorders.
Going forward with her research, Dr Morgan has three main goals she wants to achieve. First, to understand how networks change over years of duration of TLE prior to surgery. Second, to quantify exactly how networks can evolve post-surgery and lead to a resurgence in seizure activity. And finally, to combine this information into biomarkers to predict those patients with the best chance of long term seizure freedom from surgery. When these three targets are achieved, Dr Morgan believes that MRI networking mapping will be used as an effective and accurate predictive biomarker to aid treatment and help us understand this complex disease.
Reference
https://doi.org/10.33548/SCIENTIA610
Meet the researcher

Dr Victoria Lee Morgan
Professor
Department of Radiology and Radiological Sciences
Department of Biomedical Engineering
Department of Neurology
Department of Neurological Surgery
Vanderbilt University Medical Center, Nashville
Tennessee, TN
USA
Dr Victoria Morgan is a biomedical engineer with expertise in functional magnetic resonance imaging. She graduated from Wright State University in 1990 with a BSc in Biomedical Engineering before going on to earn her masters and doctorate degrees from Vanderbilt University in the same subject. In 1999, Dr Morgan joined the Vanderbilt University faculty and currently holds posts as professor of Radiology and Radiological Sciences, Biomedical Engineering, Neurology, and Neurological Surgery. Her main research focus is on designing methods to quantify networks in patients with epilepsy to improve treatment outcomes. She is a Fellow of the American Institute for Medical and Biological Engineering, a Distinguished Investigator of the Academy for Radiological and Biomedical Imaging Research, and a Fellow of the American Epilepsy Society.
CONTACT
E: victoria.morgan@vanderbilt.edu
W: https://my.vanderbilt.edu/vlmorgan/
Twitter: @VickyLMorgan
KEY COLLABORATORS
Dario J. Englot, MD, PhD, Vanderbilt University Medical Center
Baxter P. Rogers, PhD, Vanderbilt University Medical Center
Bennett A. Landman, PhD, Vanderbilt University
Bassel Abou-Khalil, MD, Vanderbilt University Medical Center
Catie Chang, PhD, Vanderbilt University
FUNDING
Current:
National Institutes of Health: 1R01NS110130. The Role of Network Connectivity in Post-Surgical Seizure Recurrence in Temporal Lobe Epilepsy
National Institutes of Health: 1R01NS108445. MRI Connectivity Biomarkers of Treatment Response in Focal Epilepsy
Past:
Epilepsy Foundation Research Grant: Localization of Epileptic Activity Using Resting Functional MRI
National Institutes of Health: 1R01 NS055822-01A2. Temporal Clustering Analysis for Detection of Irregular Transient fMRI Activation
National Institutes of Health: 1R01NS075270-01A1. MRI Structural and Functional Connectivity Changes in Temporal Lobe Epilepsy
FURTHER READING
VL Morgan, BP Rogers, AW Anderson, et al, Divergent network properties that predict early surgical failure versus late recurrence in temporal lobe epilepsy, Journal of Neurosurgery, 2020, 132(5), 1324–1333.
VL Morgan, DJ Englot, BP Rogers, et al, Magnetic resonance imaging connectivity for the prediction of seizure outcome in temporal lobe epilepsy, Epilepsia, 2017, 58(7), 1251–60.
Want to republish our articles?
We encourage all formats of sharing and republishing of our articles. Whether you want to host on your website, publication or blog, we welcome this. Find out more
Creative Commons Licence
(CC BY 4.0)
This work is licensed under a Creative Commons Attribution 4.0 International License. 
What does this mean?
Share: You can copy and redistribute the material in any medium or format
Adapt: You can change, and build upon the material for any purpose, even commercially.
Credit: You must give appropriate credit, provide a link to the license, and indicate if changes were made.
More articles you may like
Grandmothers: Innovation Through Tradition
Grandmother Project – Change through Culture (GMP) is an organisation dedicated to documenting the role of grandmothers and demonstrating the effectiveness of grandmother-inclusive strategies in improving the health and well-being of women, children, and adolescents. GMP’s groundbreaking work challenges conventional wisdom to transform community-based interventions in Africa and beyond, harnessing a powerful but often overlooked resource: the wisdom and influence of grandmothers.
Dr Robert Larkin | Cultivating Change to Improve Soil Health and Increase Potato Yield
Environmental quality and food production are facing the pressing challenges of climate change and global population growth. Dr Robert Larkin from the United States Department of Agriculture-Agricultural Research Service (USDA-ARS) and a team of plant scientists developed and tested a range of crop management systems to help overcome these compounding challenges. Their work is improving soil health and increasing the yield of potato crops, contributing to the future food security of nations.
Professor Giorgio Buttazzo | Artificial Intelligence and a Crossroads for Humanity
Where do we stand with artificial intelligence? Might machines take over our jobs? Can machines become conscious? Might we be harmed by robots? What is the future of humanity? Professor Giorgio Buttazzo of Scuola Superiore Sant’Anna is an expert in artificial intelligence and neural networks. In a recent publication, he provides considered insights into some of the most pressing questions surrounding artificial intelligence and humanity.
Dr Ralf Adam | New Technologies Shaping the Future of Oral Hygiene
Understanding the efficiency of various toothbrush technologies is essential for achieving optimal oral health. Dr Ralf Adam, who leads a dedicated team at Procter & Gamble in Germany, is keen to investigate the complexities of these technologies. His team have provided new insights into the best toothbrush types for plaque removal and the maintenance of gum health. By highlighting the importance of informed oral care decisions and ongoing investigations, this vital research works towards ensuring everyone can achieve a brighter, healthier smile.




